10-K: Annual report pursuant to Section 13 and 15(d)
Published on February 17, 2022
UNITED STATES SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM
For the fiscal year ended
For the transition period from to
(Exact Name of Registrant as Specified in its Charter)
(Omega Healthcare Investors, Inc.) |
(Omega Healthcare Investors, Inc.) |
(Omega Healthcare Investors, Inc.) |
(State or other jurisdiction of incorporation or organization) |
(Commission file number) |
(IRS Employer Identification No.) |
(Address of principal executive offices)
(
(Telephone number, including area code)
Securities Registered Pursuant to Section 12(b) of the Act:
Registrant |
|
Title of Each Class |
Trading Symbol (s) |
Name of Exchange on |
|
Omega Healthcare Investors, Inc. |
Securities registered pursuant to Section 12(g) of the Act:
None.
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act.
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act.
Yes ◻ |
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding twelve months (or for such shorter period that the registrant was required to file such reports) and (2) has been subject to such filing requirements for the past 90 days.
Indicate by check mark whether the registrant has submitted electronically, every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit such files).
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act. (Check one:)
Accelerated filer ◻ |
Non-accelerated filer ◻ |
|
Smaller reporting company ◻ |
Emerging growth company ◻ |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 7(a)(2)(B) of the Securities Act.
|
Yes
|
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C 7262(b)) by the registered public accounting firm that prepared or issued its audit report.
Yes
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act).
Yes |
The aggregate market value of the common stock Omega Healthcare Investors, Inc. held by non-affiliates was $
As of February 11, 2022, there were
DOCUMENTS INCORPORATED BY REFERENCE
Proxy Statement for the registrant’s 2022 Annual Meeting of Stockholders to be filed with the Securities and Exchange Commission no later than 120 days after December 31, 2021, is incorporated by reference in Part III herein.
TABLE OF CONTENTS
2
Forward-Looking Statements
Unless otherwise indicated or except where the context otherwise requires, the terms “we,” “us” and “our” and other similar terms in this Annual Report on Form 10-K refer to Omega Healthcare Investors, Inc. and its consolidated subsidiaries.
The following discussion should be read in conjunction with the financial statements and notes thereto appearing elsewhere in this document. This document contains “forward-looking statements” within the meaning of the federal securities laws. These statements relate to our expectations, beliefs, intentions, plans, objectives, goals, strategies, future events, performance and underlying assumptions and other statements other than statements of historical facts. In some cases, you can identify forward-looking statements by the use of forward-looking terminology including, but not limited to, terms such as “may,” “will,” “anticipates,” “expects,” “believes,” “intends,” “should” or comparable terms or the negative thereof. These statements are based on information available on the date of this filing and only speak as to the date hereof and no obligation to update such forward-looking statements should be assumed.
Our actual results may differ materially from those reflected in the forward-looking statements contained herein as a result of a variety of factors, including, among other things:
| (1) | those items discussed under “Risk Factors” in Part I, Item 1A to our Annual Report on Form 10-K; |
| (2) | uncertainties relating to the business operations of the operators of our assets, including those relating to reimbursement by third-party payors, regulatory matters and occupancy levels; |
| (3) | the impact of the COVID-19 pandemic on our business and the business of our operators, including without limitation, the extent and duration of the COVID-19 pandemic, increased costs, staffing shortages and decreased occupancy levels experienced by operators of skilled nursing facilities (“SNFs”) and assisted living facilities (“ALFs”) in connection therewith, the ability of operators to comply with infection control and vaccine protocols, the long-term impact of vaccination on facility infection rates, and the extent to which continued government support may be available to operators to offset such costs and the conditions related thereto; |
| (4) | the ability of our operators in bankruptcy to reject unexpired lease obligations, modify the terms of our mortgages and impede the ability to collect unpaid rent or interest during the pendency of a bankruptcy proceeding and retain security deposits for the debtor’s obligations, and other costs and uncertainties associated with operator bankruptcies; |
| (5) | our ability to re-lease, otherwise transition, or sell underperforming assets or assets held for sale on a timely basis and on terms that allow us to realize the carrying value of these assets; |
| (6) | the availability and cost of capital to us; |
| (7) | changes in our credit ratings and the ratings of our debt securities; |
| (8) | competition in the financing of healthcare facilities; |
| (9) | competition in the long-term healthcare industry and shifts in the perception of various types of long-term care facilities, including SNFs and ALFs; |
| (10) | additional regulatory and other changes in the healthcare sector; |
| (11) | changes in the financial position of our operators; |
| (12) | the effect of economic and market conditions generally and, particularly, in the healthcare industry; |
| (13) | changes in interest rates; |
| (14) | the timing, amount and yield of any additional investments; |
| (15) | changes in tax laws and regulations affecting real estate investment trusts (“REITs”); |
| (16) | the potential impact of changes in the SNF and ALF markets or local real estate conditions on our ability to dispose of assets held for sale for the anticipated proceeds or on a timely basis, or to redeploy the proceeds therefrom on favorable terms; |
| (17) | our ability to maintain our status as a REIT; and |
| (18) | the effect of other factors affecting our business or the businesses of our operators that are beyond our or their control, including natural disasters, other health crises or pandemics and governmental action; particularly in the healthcare industry. |
3
PART I
Item 1 – Business
Overview
Omega Healthcare Investors, Inc. (“Parent”) is a Maryland corporation that, together with its consolidated subsidiaries (collectively, “Omega” or “Company”) has elected to be taxed as a REIT for federal income tax purposes. Omega is structured as an umbrella partnership REIT (“UPREIT”) under which all of Omega's assets are owned directly or indirectly by, and all of Omega's operations are conducted directly or indirectly through, its operating partnership subsidiary, OHI Healthcare Properties Limited Partnership (collectively with subsidiaries, “Omega OP”). As of December 31, 2021, Parent owned approximately 97% of the issued and outstanding units of partnership interest in Omega OP (“Omega OP Units”), and other investors owned approximately 3% of the outstanding Omega OP Units. Omega became a publicly traded company listed on the New York Stock Exchange in 1992.
Omega has one reportable segment consisting of investments in healthcare-related real estate properties located in the United States (“U.S.”) and the United Kingdom (“U.K.”). Our core business is to provide financing and capital to the long-term healthcare industry with a particular focus on skilled nursing facilities (“SNFs”), assisted living facilities (“ALFs”), and to a lesser extent, independent living facilities (“ILFs”), rehabilitation and acute care facilities (“specialty facilities”) and medical office buildings (“MOBs”). Our core portfolio consists of our long-term leases and mortgage loans with healthcare operating companies and affiliates (collectively, our “operators”). All of our leases to our operators are “triple-net” leases, which require the operators to pay all property-related expenses. All of our mortgages are secured by first mortgage liens on the underlying real estate and personal property of the operators. In addition to our core investments, we selectively make loans to operators for working capital and capital expenditures. These loans, which may be either unsecured or secured by the collateral of the borrower, are classified as other investments. From time to time, we also acquire equity interests in joint ventures or entities that support the long-term healthcare industry and our operators.
Our goal is to provide strong returns to our investors, while serving as the preferred capital partner to our operators so they can concentrate on providing a high level of care for their resident-patients.
Portfolio and Investments
As of December 31, 2021, our portfolio of real estate investments included 960 healthcare facilities located in 42 states and the U.K. and operated by 63 third-party operators and was made up of the following:
| ● | real estate assets that include 685 SNFs, 133 ALFs, 20 ILFs, 16 specialty facilities and two MOBs; |
| ● | fixed rate mortgages on 59 SNFs, two ALFs and two specialty facilities; and |
| ● | 41 facilities held for sale. |
Included below is a summary of our total investment assets, excluding accumulated depreciation, as of December 31, 2021 and 2020 (dollars in thousands):
As of December 31, |
||||||
|
2021 |
|
2020 |
|||
Real estate assets: |
||||||
Buildings and improvements |
$ |
7,448,126 |
$ |
7,269,596 |
||
Land |
|
916,328 |
|
883,765 |
||
Furniture and equipment |
|
511,271 |
|
518,664 |
||
Construction in progress |
|
74,062 |
|
30,129 |
||
Total real estate assets |
|
8,949,787 |
|
8,702,154 |
||
Investments in direct financing leases - net |
|
10,873 |
|
10,764 |
||
Mortgage notes receivable - net |
|
835,086 |
|
885,313 |
||
Assets held for sale |
|
261,151 |
|
81,452 |
||
Total real estate investments |
|
10,056,897 |
|
9,679,683 |
||
Other investments - net |
|
469,884 |
|
467,442 |
||
Investments in unconsolidated joint ventures |
|
194,687 |
|
200,638 |
||
Total investments |
$ |
10,721,468 |
$ |
10,347,763 |
||
4
Revenues
The following table summarizes our revenues by investment category for 2021, 2020 and 2019 (dollars in thousands):
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
|
2019 |
||||
Real estate related income: |
|||||||||
Rental income |
$ |
923,677 |
$ |
753,427 |
$ |
804,076 |
|||
Income from direct financing leases |
|
1,029 |
|
1,033 |
|
1,036 |
|||
Mortgage interest income |
|
91,661 |
|
89,422 |
|
76,542 |
|||
Total real estate related revenues |
|
1,016,367 |
|
843,882 |
|
881,654 |
|||
Other investment income |
|
44,721 |
|
44,864 |
|
43,400 |
|||
Miscellaneous income |
|
1,721 |
|
3,635 |
|
3,776 |
|||
Total revenues |
$ |
1,062,809 |
$ |
892,381 |
$ |
928,830 |
|||
Investment Strategy
We maintain a portfolio of long-term healthcare facilities and mortgages on healthcare facilities located in the U.S. and the U.K. Our investments are generally geographically diverse and operated by a diverse group of established, middle-market healthcare operators that we believe meet our standards for quality and experience of management and creditworthiness. Our criteria for evaluating potential investments includes but is not limited to:
● the quality and experience of management and the creditworthiness of the operator of the facility;
● the facility’s historical and forecasted cash flow and its ability to meet operational needs, capital expenditure requirements and lease or debt service obligations;
● the construction quality, condition and design of the facility and its environmental impact;
● the location of the facility;
● the tax, growth, regulatory and reimbursement environment of the applicable jurisdiction;
● the occupancy rate for the facility and demand for similar healthcare facilities in the same or nearby communities; and
● the payor mix of private, Medicare and Medicaid patients at the facility.
As healthcare delivery continues to evolve, we continuously evaluate potential investments, as well as our assets, operators and markets to position our portfolio for long-term success. Our strategy includes applying data analytics to our investment underwriting and asset management, as well as selling or transitioning assets that do not meet our portfolio criteria.
We prefer to invest in fee simple ownership of properties. Due to regulatory, tax or other considerations, we may pursue alternative investment structures, such as mortgages and investments in joint ventures. While the market for long-term care real estate acquisitions in the U.S. remained competitive in 2021, we continued to seek and identify selective investments that are accretive to our portfolio. In addition to our U.S.-based investments, we expect to continue to pursue investments in alternative jurisdictions such as the U.K. As part of our continuous evaluation of our portfolio and in connection with certain operator workout transactions, we expect to continue to opportunistically sell assets, or portfolios of assets, from time to time. In addition, as the long-term care industry evolves and adapts to new protocols, we have made and may continue to make select ancillary investments in companies that enhance the technology and infrastructure of long-term care providers and our operators.
The following summarizes our primary investment structures. The average annualized yields described below reflect obligations under existing contractual arrangements. However, due to the nature of the long-term care industry, we cannot assure that the operators of our facilities will meet their payment obligations in full or when due. Therefore, the annualized yields as of December 31, 2021, set forth below, are not necessarily indicative of future yields, which may be lower.
We seek to obtain (i) contractual rent escalations under long-term, non-cancelable, “triple-net” leases and (ii) fixed-rate mortgage loans. We also typically seek to obtain substantial liquidity deposits, covenants regarding minimum working capital and net worth, liens on accounts receivable and other operating assets, and various provisions for cross-default, cross-collateralization and corporate and/or personal guarantees, when appropriate.
5
Triple-Net Operating Leases
Our triple-net operating leases typically range from 5 to 15 years, plus renewal options and require the operator to pay rent and all additional charges incurred in the operation of the leased facility. Our leases generally provide for minimum annual rents that are subject to annual escalators. Leases with fixed annual rental escalators are generally recognized on a straight-line basis over the initial lease period, subject to a collectibility assessment. At December 31, 2021, our average annualized yield from operating leases was approximately 9.8%. At December 31, 2021, approximately 94% of our operating leases have initial lease terms expiring after 2026. The majority of our leased real estate properties are leased under provisions of master lease agreements that govern more than one facility and to a lesser extent we lease facilities under single facility leases. Under our master leases, our operators are required to make one monthly payment that represents rent on all the properties that are subject to the master lease.
Some of our leases provide our operators with advances for the construction of facilities or capital expenditures for strategic facility enhancements. Typically, these advances require the operator to pay a fixed percentage of the advances funded as capital expenditure rent under the lease. Construction and upgrades made under these lease clauses are capitalized within our real estate assets. Because we direct a significant amount of our capital back into existing assets, we believe this sets the stage for our long-term strategic success.
Fixed-Rate Mortgages
Our mortgages typically have a fixed interest rate for the mortgage term and are secured by first mortgage liens on the underlying real estate and personal property of the mortgagor. We enter into mortgages for existing facilities and for the construction of facilities. At December 31, 2021, our average annualized yield on these investments was approximately 10.5%. At December 31, 2021, approximately 89% of our mortgages have primary terms that expire after 2026.
The table set forth in Item 2 – Properties contains information regarding our properties and investments as of December 31, 2021.
Borrowing Policies
We generally attempt to match the maturity of our indebtedness with the maturity of our investment assets and employ long-term, fixed-rate debt to the extent practicable in view of market conditions in existence from time to time.
We may use the proceeds of new indebtedness to finance our investments in additional healthcare facilities. In addition, we may invest in properties subject to existing loans, secured by mortgages, deeds of trust or similar liens on properties.
Policies With Respect To Certain Activities
With respect to our capital requirements, we typically rely on equity offerings, debt financing and retention of cash flow (subject to provisions in the Internal Revenue Code of 1986, as amended (the “Code”) concerning taxability of undistributed REIT taxable income), or a combination of these methods. Our financing alternatives include bank borrowings, publicly or privately placed debt instruments, purchase money obligations to the sellers of assets or securitizations, any of which may be issued as secured or unsecured indebtedness. We have the authority to issue our common stock or other equity or debt securities in exchange for property and to repurchase or otherwise reacquire our securities. Subject to the percentage of ownership limitations and gross income and asset tests necessary for REIT qualification, we may invest in securities of other REITs, other entities engaged in real estate activities or securities of other issuers, including for the purpose of exercising control over such entities. We may engage in the purchase and sale of investments. We do not underwrite the securities of other issuers. Our officers and directors may change any of these policies without a vote of our stockholders. In the opinion of our management, our properties are adequately covered by insurance.
6
Competition
The healthcare industry is highly competitive and will likely become more competitive in the future. We face competition in making and pricing new investments from other public and private REITs, investment companies, private equity and hedge fund investors, healthcare operators, lenders, developers and other institutional investors, some of whom may have greater resources and lower costs of capital than us. We believe our use of data analytics to underwrite investments and manage our portfolio may provide us a competitive advantage. In addition, a significant amount of our rental and mortgage income is generally derived from facilities in states that require state approval for development and expansion of healthcare facilities. We believe that such state approvals may reduce competition for our operators and enhance the value of our properties. Our operators compete on a local and regional basis with operators of facilities that provide comparable services. The basis of competition for our operators includes, amongst other factors, the quality of care provided, reputation, the physical appearance of a facility, price, the range of services offered, family preference, alternatives for healthcare delivery, the supply of competing properties, physicians, staff, referral sources, location and the size and demographics of the population and surrounding areas.
Increased competition makes it more challenging for us to identify and successfully capitalize on opportunities that meet our objectives. Our ability to compete is also impacted by national and local economic trends, availability of investment alternatives, availability and cost of capital, construction and renovation costs, existing laws and regulations, new legislation and population trends.
Taxation of Omega
Omega elected to be taxed as a REIT, under Sections 856 through 860 of the Code, beginning with our taxable year ended December 31, 1992. To continue to qualify as a REIT, we must continue to meet certain tests that, among other things, generally require that our assets consist primarily of real estate assets, our income be derived primarily from real estate assets, and that we distribute at least 90% of our REIT taxable income (other than net capital gains) to our stockholders annually. Provided we maintain our qualification as a REIT, we generally will not be subject to U.S. federal income taxes at the corporate level on our net income to the extent such net income is distributed to our stockholders annually. Even if we continue to qualify as a REIT, we will continue to be subject to certain federal, state and local taxes on our income and property. We believe that we were organized and have operated in such a manner as to qualify for taxation as a REIT. We intend to continue to operate in a manner that will allow us to maintain our qualification as a REIT, but no assurance can be given that we have operated or will be able to continue to operate in a manner so as to qualify or remain qualified as a REIT.
We have utilized, and may continue to utilize, one or more taxable REIT subsidiary (“TRS”) to engage in activities that REITs may be prohibited from performing, including the provision of management and other services to third parties and the conduct of certain nonqualifying real estate transactions. Our TRSs generally are taxable as regular corporations, and therefore, subject to federal, foreign, state and local income taxes.
To the extent that we do not distribute all of our net capital gain or do distribute at least 90%, but less than 100% of our “REIT taxable income,” as adjusted, we will be subject to tax thereon at regular ordinary and capital gain corporate tax rates. If we were to fail to qualify as a REIT in any taxable year, as a result of a determination that we failed to meet the annual distribution requirement or otherwise, we would be subject to federal and state income tax, and any applicable alternative minimum tax on our taxable income at regular corporate rates with respect to each such taxable year for which the statute of limitations remains open. In addition, even if we continue to qualify as a REIT, we could become subject to certain excise taxes. Moreover, unless entitled to relief under certain statutory provisions, we also would be disqualified from treatment as a REIT for the four taxable years following the year during which qualification is lost. This treatment would significantly reduce our net earnings and cash flow because of our additional tax liability for the years involved, which could significantly impact our financial condition.
7
All of our investments are held directly or through entities owned by Omega OP. Omega OP is a pass through entity for U.S. federal income tax purposes, and therefore we are required to take into account our allocable share of each item of Omega OP’s income, gain, loss, deduction, and credit for any taxable year of Omega OP ending within or with our taxable year, without regard to whether we have received or will receive any distribution from Omega OP. Although a partnership agreement for pass through entities generally will determine the allocation of income and losses among partners, such allocations will be disregarded for tax purposes if they do not comply with the provisions of the Code and Treasury Regulations governing partnership allocations. If an allocation is not recognized for federal income tax purposes, the item subject to the allocation will be reallocated in accordance with the partners’ interests in the partnership, which will be determined by considering all the facts and circumstances relating to the economic arrangement of the partners with respect to such item. While Omega OP should generally not be a taxable entity for federal income tax purposes, any state or local revenue, excise or franchise taxes that result from the operating activities of the Omega OP may be incurred at the entity level.
Investors are strongly urged to consult their own tax advisors regarding the potential tax consequences of an investment in us based on such investor’s particular circumstances.
Government Regulation and Reimbursement
The healthcare industry is heavily regulated. Our operators, which are primarily based in the U.S., are subject to extensive and complex federal, state and local healthcare laws and regulations; we also have several U.K.-based operators that are impacted by a variety of laws and regulations in their jurisdiction. These laws and regulations are subject to frequent and substantial changes resulting from the adoption of new legislation, rules and regulations, and administrative and judicial interpretations of existing law. The ultimate timing or effect of these changes, which may be applied retroactively, cannot be predicted. Changes in laws and regulations impacting our operators, in addition to regulatory non-compliance by our operators, can have a significant effect on the operations and financial condition of our operators, which in turn may adversely impact us. There is the potential that we may be subject directly to healthcare laws and regulations because of the broad nature of some of these regulations, such as the Anti-kickback Statute and False Claims Act, among others.
The U.S. Department of Health and Human Services (“HHS”) declared a public health emergency on January 31, 2020 following the World Health Organization's decision to declare COVID-19 a public health emergency of international concern. This declaration, which has been extended through April 14, 2022, allows HHS to provide temporary regulatory waivers and new reimbursement rules designed to equip providers with flexibility to respond to the COVID-19 pandemic by suspending various Medicare patient coverage criteria and documentation and care requirements, including, for example, suspension of the three-day prior hospital stay coverage requirement and expanding the list of approved services which may be provided via telehealth. These regulatory actions have contributed, and may continue to contribute, to a change in census volumes and skilled nursing mix that may not otherwise have occurred. It remains uncertain when federal and state regulators will resume enforcement of those regulations which are waived or otherwise not being enforced during the public health emergency due to the exercise of enforcement discretion.
These temporary changes to regulations and reimbursement, as well as emergency legislation, including the CARES Act enacted on March 27, 2020 and discussed below, continue to have a significant impact on the operations and financial condition of our operators. The extent of the COVID-19 pandemic’s effect on the Company’s and our operators’ operational and financial performance will depend on future developments, including the sufficiency and timeliness of additional governmental relief, the duration, spread and intensity of the outbreak, the impact of genetic mutations of the virus into new variants, the impact of vaccine distributions and booster doses on our operators and their populations, the impact of vaccine mandates on staffing shortages at our operators, as well as the difference in how the pandemic may impact SNFs in contrast to ALFs, all of which developments and impacts are uncertain and difficult to predict. Due to these uncertainties, we are not able at this time to estimate the effect of these factors on our business; however, the adverse impact on our business, results of operations, financial condition and cash flows could be material.
8
A significant portion of our operators’ revenue is derived from government-funded reimbursement programs, consisting primarily of Medicare and Medicaid. As federal and state governments continue to focus on healthcare reform initiatives, efforts to reduce costs by government payors will likely continue. Significant limits on the scope of services reimbursed and/or reductions of reimbursement rates could therefore have a material adverse effect on our operators’ results of operations and financial condition. Additionally, new and evolving payor and provider programs that are tied to quality and efficiency could adversely impact our tenants’ and operators’ liquidity, financial condition or results of operations, and there can be no assurance that payments under any of these government healthcare programs are currently, or will be in the future, sufficient to fully reimburse the property operators for their operating and capital expenses. In addition to quality and value based reimbursement reforms, the U.S. Centers for Medicare and Medicaid Services (“CMS”) has implemented a number of initiatives focused on the reporting of certain facility specific quality of care indicators that could affect our operators, including publicly released quality ratings for all of the nursing homes that participate in Medicare or Medicaid under the CMS “Five Star Quality Rating System.” Facility rankings, ranging from five stars (“much above average”) to one star (“much below average”) are updated on a monthly basis. SNFs are required to provide information for the CMS Nursing Home Compare website regarding staffing and quality measures. These rating changes have impacted referrals to SNFs, and it is possible that changes to this system or other ranking systems could lead to future reimbursement policies that reward or penalize facilities on the basis of the reported quality of care parameters.
The following is a discussion of certain U.S. laws and regulations generally applicable to our operators, and in certain cases, to us.
Reimbursement Changes Related to COVID-19:
U.S. Federal Stimulus Funds and Financial Assistance for Healthcare Providers. In response to the pandemic, Congress has enacted a series of economic stimulus and relief measures. On March 18, 2020, the Families First Coronavirus Response Act was enacted in the U.S., providing a temporary 6.2% increase to each qualifying state and territory’s Medicaid Federal Medical Assistance Percentage (“FMAP”) effective January 1, 2020. The temporary FMAP increase will extend through the last day of the calendar quarter in which the public health emergency terminates. States will make individual determinations about how this additional Medicaid reimbursement will be applied to SNFs, if at all.
In further response to the pandemic, in 2020, the CARES Act authorized approximately $178 billion to be distributed through the Provider Relief Fund to reimburse eligible healthcare providers for healthcare related expenses or lost revenues that are attributable to coronavirus. In addition, in September 2021, HHS announced the release of $25.5 billion in provider funding, including $17 billion of the $178 billion previously authorized through the CARES Act and $8.5 billion for rural providers through the American Rescue Plan Act. The Provider Relief Fund is administered under the broad authority and discretion of HHS and recipients are not required to repay distributions received to the extent they are used in compliance with applicable requirements.
HHS began distributing Provider Relief Fund grants in April 2020 and has made grants available to various provider groups in four general phases. In May 2020, HHS announced that approximately $9.5 billion in targeted distributions would be made available to eligible SNFs, approximately $2.5 billion of which were composed of performance-based incentive payments tied to a facility’s infection rate. Approximately $8.5 billion in additional funds were added to the Provider Relief Fund through the American Rescue Plan Act enacted on March 11, 2021; however, these funds are limited to rural providers and suppliers. In September 2021, HHS announced the release of $25.5 billion of funding, including $17 billion in Phase 4 Provider Relief Fund payments for a broad range of healthcare providers who can document revenue loss and expenses associated with the pandemic between July 1, 2020 and March 31, 2021, as well as release of the $8.5 billion in funding for rural providers, including those with Medicaid and Medicare patients. In addition, in September 2021, the Centers for Disease Control and Prevention (“CDC”) announced it would allocate $500 million to staffing, training and deployment of state-based nursing home and long-term care “strike teams” to assist facilities with known or suspected COVID-19 outbreaks.
HHS continues to evaluate and provide allocations of, and issue regulation and guidance regarding, grants made under the CARES Act. There are substantial uncertainties regarding the extent to which our operators will receive additional funding from HHS.
9
The CARES Act and related legislation also made other forms of financial assistance available to healthcare providers, which have the potential to impact our operators to varying degrees. This assistance includes Medicare and Medicaid payment adjustments and an expansion of the Medicare Accelerated and Advance Payment Program, which made available accelerated payments of Medicare funds in order to increase cash flow to providers. These payments are loans that providers are scheduled to repay beginning one year from the issuance date of each provider’s or supplier’s accelerated or advance payment, with repayment made through automatic recoupment of 25% of Medicare payments otherwise owed to the provider or supplier for eleven months, followed by an increase to 50% for another six months, after which any outstanding balance would be repaid subject to an interest rate of 4%. We believe these repayments commenced for many of our operators in April 2021 and have adversely impacted, and will continue to adversely impact, operating cash flows of these operators.
Additionally, CMS suspended Medicare sequestration payment adjustments, which would have otherwise reduced payments to Medicare providers by 2%, from May 1, 2020 through December 31, 2020, but also extended sequestration through 2030. The Bipartisan-Bicameral Omnibus COVID Relief Deal passed in December 2020 further extended the suspension of the Medicare sequestration until March 31, 2021, and it most recently has been further extended from December 31, 2021 through March 31, 2022. While not limited to healthcare providers, the CARES Act additionally provided payroll tax relief for employers, allowing them to defer payment of employer Social Security taxes that are otherwise owed for wage payments made after March 27, 2020 through December 31, 2020 to December 31, 2021 with respect to 50% of the payroll taxes owed, with the remaining 50% deferred until December 31, 2022.
Quality of Care Initiatives and Additional Requirements Related to COVID-19. In addition to COVID-19 reimbursement changes, several regulatory initiatives announced in 2020 and 2021 focused on addressing quality of care in long-term care facilities, including those related to COVID-19 testing and infection control protocols, vaccine protocols, staffing levels, reporting requirements, and visitation policies, as well as increased inspection of nursing homes. In August 2021, CMS announced it was developing an emergency regulation requiring staff vaccinations within the nation’s more than 15,000 Medicare and Medicaid-participating nursing homes, and in September 2021, CMS further announced that the scope of the regulation will be expanded to include workers in hospitals, dialysis facilities, ambulatory surgical settings, and home health agencies. In addition, recent updates to the Nursing Home Care website and the Five Star Quality Rating System include revisions to the inspection process, adjustment of staffing rating thresholds, the implementation of new quality measures and the inclusion of a staff turnover percentage (over a 12-month period). Although the American Rescue Plan Act did not allocate specific funds to SNF or ALF providers, approximately $200 million was allocated to quality improvement organizations to provide infection control and vaccination uptake support to SNFs and $500 million has been allocated by the CDC to staffing, training and deployment of state-based nursing home and long-term care “strike teams” to assist facilities with known or suspected COVID-19 outbreaks.
On June 16, 2020, the U.S. House of Representatives Select Subcommittee on the Coronavirus Crisis announced the launch of an investigation into the COVID-19 response of nursing homes and the use of federal funds by nursing homes during the pandemic. The Select Subcommittee continued to be active throughout the remainder of 2020 and 2021. In March 2021, the Oversight Subcommittee of the House Ways and Means Committee held a hearing on examining the impact of private equity in the U.S. healthcare system, including the impact on quality of care provided within the skilled nursing industry. These hearings, as well as additional calls for government review of the role of private equity in the U.S. healthcare industry, could result in legislation imposing additional requirements on our operators.
10
Reimbursement Generally:
Medicaid. The American Rescue Plan Act contains several provisions designed to increase coverage, expand benefits, and adjust federal financing for state Medicaid programs. For example, the American Rescue Plan Act increases the FMAP by 10 percentage points for state home and community-based services expenditures beginning April 1, 2021 through March 30, 2022 in an effort to assist seniors and people with disabilities to receive services safely in the community rather than in nursing homes and other congregate care settings. As a condition for receiving the FMAP increase, states must enhance, expand, or strengthen their Medicaid home and community-based services program during this period. These potential enhancements to Medicaid reimbursement funding may be offset in certain states by state budgetary concerns, the ability of the state to allocate matching funds and to comply with the new requirements, the potential for increased enrollment in Medicaid due to unemployment and declines in family incomes resulting from the COVID-19 pandemic, and the potential allocation of state Medicaid funds available for reimbursement away from SNFs in favor of home and community-based programs. These challenges may particularly impact us in states where we have a larger presence, including Florida and Texas. In Texas in particular, several of our operators have historically experienced lower operating margins on their SNFs, as compared to other states, as a result of lower Medicaid reimbursement rates and higher labor costs. Our operators in Texas may also be adversely impacted by the expected expiration of an add-on by the state to the daily reimbursement rate for Medicaid patients that will terminate upon expiration of the federally declared public health emergency. In Florida, while added support to our operators during the pandemic has generally been limited, approximately $100 million in additional FMAP funds for nursing homes was approved by the State in November 2021, with the funds to be distributed through increased Medicaid payment rates over a three-month period. Since our operators’ profit margins on Medicaid patients are generally relatively low, more than modest reductions in Medicaid reimbursement or an increase in the percentage of Medicaid patients has in the past and may in the future adversely affect our operators’ results of operations and financial condition, which in turn could adversely impact us.
Medicare. On July 29, 2021, CMS issued a final rule regarding the government fiscal year 2022 Medicare payment rates and quality payment programs for SNFs, with aggregate Medicare Part A payments projected to increase by $410 million, or 1.2%, for fiscal year 2022 compared to fiscal year 2021. This estimated reimbursement increase is attributable to a 2.7% market basket increase factor less a 0.8 percentage point forecast error adjustment and a 0.7 percentage point productivity adjustment, and a $1.2 million decrease due to the proposed reduction to the SNF prospective payment system rates to account for the recent blood-clotting factors exclusion. The annual update is reduced by two percentage points for SNFs that fail to submit required quality data to CMS under the SNF Quality Reporting Program. CMS has indicated that these impact figures did not incorporate the SNF Value-Based Program reductions that are estimated to be $184.25 million in fiscal year 2022.
Payments to providers continue to be increasingly tied to quality and efficiency. The Patient Driven Payment Model (“PDPM”), which was designed by CMS to improve the incentives to treat the needs of the whole patient, became effective October 1, 2019. Prior to COVID-19, we believed that certain of our operators could realize efficiencies and cost savings from increased concurrent and group therapy under PDPM and some had reported early positive results. Given the ongoing impacts of COVID-19, many operators are and may continue to be restricted from pursuing concurrent and group therapy and unable to realize these benefits. Additionally, our operators continue to adapt to the reimbursement changes and other payment reforms resulting from the value based purchasing programs applicable to SNFs under the 2014 Protecting Access to Medicare Act. These reimbursement changes have had and may, together with any further reimbursement changes to PDPM or value-based purchasing models, in the future have an adverse effect on the operations and financial condition of some operators and could adversely impact the ability of operators to meet their obligations to us.
On May 27, 2020, CMS added physical therapy, occupational therapy and speech-language pathology to the list of approved telehealth Providers for the Medicare Part B programs provided by a SNF as a part of the COVID-19 1135 waiver provisions. The COVID-19 1135 waiver provisions also allow for the facility to bill an originating site fee to CMS for telehealth services provided to Medicare Part B beneficiary residents of the facility when the services are provided by a physician from an alternate location, effective March 6, 2020 through the end of the public health emergency.
11
Other Regulation:
Office of the Inspector General Activities. The Office of Inspector General (“OIG”) of HHS has provided long-standing guidance for SNFs regarding compliance with federal fraud and abuse laws. More recently, the OIG has conducted increased oversight activities and issued additional guidance regarding its findings related to identified problems with the quality of care and the reporting and investigation of potential abuse or neglect at group homes, nursing homes and SNFs. The OIG has additionally reviewed the staffing levels reported by SNFs as part of its August 2018 and February 2019 Work Plan updates, and included a review of involuntary transfers and discharges from nursing homes in the June 2019 Work Plan updates. In August 2020, the OIG released its findings regarding its review of staffing levels in SNFs from 2018. The OIG recommended that CMS enhance efforts to ensure nursing homes meet daily staffing requirements and explore ways to provide consumers with additional information on nursing homes’ daily staffing levels and variability. The OIG indicated that while the review was initiated before the COVID-19 pandemic emerged, the pandemic reinforces the importance of sufficient staffing for nursing homes, as inadequate staffing can make it more difficult for nursing homes to respond to infectious disease outbreaks like COVID-19. It is unknown what impact, if any, enhanced scrutiny of staffing levels by OIG and CMS will have on our operators.
Department of Justice and Other Enforcement Actions. SNFs are under intense scrutiny for ensuring the quality of care being rendered to residents and appropriate billing practices conducted by the facility. The Department of Justice (“DOJ”) has historically used the False Claims Act to civilly pursue nursing homes that bill the federal government for services not rendered or care that is grossly substandard. For example, California prosecutors announced in March 2021 an investigation into a skilled nursing provider that is affiliated with one of our operators, alleging the chain manipulated the submission of staffing level data in order to improve its Five Star rating. In 2020, the DOJ launched a National Nursing Home Initiative to coordinate and enhance civil and criminal enforcement actions against nursing homes with grossly substandard deficiencies. Such enforcement activities are unpredictable and may develop over lengthy periods of time. An adverse resolution of any of these enforcement activities or investigations incurred by our operators may involve injunctive relief and/or substantial monetary penalties, either or both of which could have a material adverse effect on their reputation, business, results of operations and cash flows.
Medicare and Medicaid Program Audits. Governmental agencies and their agents, such as the Medicare Administrative Contractors, fiscal intermediaries and carriers, as well as the OIG, CMS and state Medicaid programs, conduct audits of our operators’ billing practices from time to time. CMS contracts with Recovery Audit Contractors on a contingency basis to conduct post-payment reviews to detect and correct improper payments in the fee-for-service Medicare program, to managed Medicare plans and in the Medicaid program. Regional Recovery Audit Contractor program auditors along with the OIG and DOJ are expected to continue their efforts to evaluate SNF Medicare claims for any excessive therapy charges. CMS also employs Medicaid Integrity Contractors to perform post-payment audits of Medicaid claims and identify overpayments. In addition, the state Medicaid agencies and other contractors have increased their review activities. To the extent any of our operators are found out of compliance with any of these laws, regulations or programs, their financial position and results of operations can be adversely impacted, which in turn could adversely impact us.
Fraud and Abuse. There are various federal and state civil and criminal laws and regulations governing a wide array of healthcare provider referrals, relationships and arrangements, including laws and regulations prohibiting fraud by healthcare providers. Many of these complex laws raise issues that have not been clearly interpreted by the relevant governmental authorities and courts.
These laws include: (i) federal and state false claims acts, which, among other things, prohibit providers from filing false claims or making false statements to receive payment from Medicare, Medicaid or other federal or state healthcare programs; (ii) federal and state anti-kickback and fee-splitting statutes, including the Medicare and Medicaid Anti-kickback statute, which prohibit the payment or receipt of remuneration to induce referrals or recommendations of healthcare items or services, such as services provided in a SNF; (iii) federal and state physician self-referral laws (commonly referred to as the Stark Law), which generally prohibit referrals by physicians to entities for designated health services (some of which are provided in SNFs) with which the physician or an immediate family member has a financial relationship; (iv) the federal Civil Monetary Penalties Law, which prohibits, among other things, the knowing presentation of a false or fraudulent claim for certain healthcare services and (v) federal and state privacy laws, including the privacy and security rules contained in the Health Insurance Portability and Accountability Act of 1996, which provide for the privacy and security of personal health information.
12
Violations of healthcare fraud and abuse laws carry civil, criminal and administrative sanctions, including punitive sanctions, monetary penalties, imprisonment, denial of Medicare and Medicaid reimbursement and potential exclusion from Medicare, Medicaid or other federal or state healthcare programs. Additionally, there are criminal provisions that prohibit filing false claims or making false statements to receive payment or certification under Medicare and Medicaid, as well as failing to refund overpayments or improper payments. Violation of the Anti-kickback statute or Stark Law may form the basis for a federal False Claims Act violation. These laws are enforced by a variety of federal, state and local agencies and can also be enforced by private litigants through, among other things, federal and state false claims acts, which allow private litigants to bring qui tam or whistleblower actions, which have become more frequent in recent years.
Several of our operators have responded to subpoenas and other requests for information regarding their operations in connection with inquiries by the DOJ or other regulatory agencies. In addition, MedEquities Realty Trust, Inc., which we acquired in May 2019, has responded to a Civil Investigative Demand from the DOJ in connection with Lakeway Regional Medical Center. See Note 20 – Commitments and Contingencies to the Consolidated Financial Statements.
Privacy. Our operators are subject to various federal, state and local laws and regulations designed to protect the confidentiality and security of patient health information, including the federal Health Insurance Portability and Accountability Act of 1996, as amended, the Health Information Technology for Economic and Clinical Health Act (“HITECH”), and the corresponding regulations promulgated thereunder (collectively referred to herein as “HIPAA”). The HITECH Act expanded the scope of these provisions by mandating individual notification in instances of breaches of protected health information, providing enhanced penalties for HIPAA violations, and granting enforcement authority to states’ Attorneys General in addition to the HHS Office for Civil Rights (“OCR”). Additionally, in a final rule issued in January 2013, HHS modified the standard for determining whether a breach has occurred by creating a presumption that any non-permitted acquisition, access, use or disclosure of protected health information is a breach unless the covered entity or business associate can demonstrate through a risk assessment that there is a low probability that the information has been compromised.
Various states have similar laws and regulations that govern the maintenance and safeguarding of patient records, charts and other information generated in connection with the provision of professional medical services. These laws and regulations require our operators to expend the requisite resources to secure protected health information, including the funding of costs associated with technology upgrades. Operators found in violation of HIPAA or any other privacy law or regulation may face significant monetary penalties. In addition, compliance with an operator’s notification requirements in the event of a breach of unsecured protected health information could cause reputational harm to an operator’s business.
Licensing and Certification. Our operators and facilities are subject to various federal, state and local licensing and certification laws and regulations, including laws and regulations under Medicare and Medicaid requiring operators of SNFs and ALFs to comply with extensive standards governing operations. Governmental agencies administering these laws and regulations regularly inspect our operators’ facilities and investigate complaints. Our operators and their managers receive notices of observed violations and deficiencies from time to time, and sanctions have been imposed from time to time on facilities operated by them. In addition, many states require certain healthcare providers to obtain a certificate of need, which requires prior approval for the construction, expansion or closure of certain healthcare facilities, which has the potential to impact some of our operators’ abilities to expand or change their businesses.
Other Laws and Regulations. Additional federal, state and local laws and regulations affect how our operators conduct their operations, including laws and regulations protecting consumers against deceptive practices and otherwise generally affecting our operators’ management of their property and equipment and the conduct of their operations (including laws and regulations involving fire, health and safety; the Americans with Disabilities Act (the “ADA”), which imposes certain requirements to make facilities accessible to persons with disabilities, the costs for which we may be directly or indirectly responsible; the U.S. Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively referred to as the “Healthcare Reform Law”), which amended requirements for staff training, discharge planning, infection prevention and control programs, and pharmacy services, among others; staffing; quality of services, including care and food service; residents’ rights, including abuse and neglect laws; and health standards, including those set by the federal Occupational Safety and Health Administration (in the U.S.). It is anticipated that our operators will continue to face additional federal and state regulatory requirements related to the operation of their facilities in response to the COVID-19 pandemic. These requirements may continue to evolve and develop over lengthy periods of time.
13
General and Professional Liability. Although arbitration agreements have been effective in limiting general and professional liabilities for SNF and long-term care providers, there have been numerous lawsuits in recent years challenging the validity of arbitration agreements in long-term care settings. On July 16, 2019, CMS issued a final rule lifting the prohibition on pre-dispute arbitration agreements offered to residents at the time of admission provided that certain requirements are met. The rule prohibits providers from requiring residents to sign binding arbitration agreements as a condition for receiving care and requires that the agreements specifically grant residents the explicit right to rescind the agreement within thirty calendar days of signing. A number of professional liability and employment related claims have been filed or are threatened to be filed against long-term care providers related to COVID-19. While such claims may be subject to liability protection provisions within various state executive orders or legislation and/or federal legislation, an adverse resolution of any of legal proceeding or investigations against our operators may involve injunctive relief and/or substantial monetary penalties, either or both of which could have a material adverse effect on our operators’ reputation, business, results of operations and cash flows.
U.K. Regulations. The U.K. also imposes very high levels of regulation on our U.K.-based operators. In England, where all of our operators are based, the Care Quality Commission has regulatory oversight authority over the health and social care sectors and is responsible for approving, registering and inspecting our operators and the properties where they provide services. There is also a detailed legislative and regulatory framework in the U.K. designed to protect the vulnerable (whether by virtue of age or physical and/or mental impairment) and to prevent abuse. Each of these regulatory regimes carries significant enforcement powers, including the ability to criminally prosecute offending operators and facilities, impose fines or revoke registrations. Additionally, under the purview of the Competition and Markets Authority, local authorities are tasked with providing and funding the care needs of eligible residents within the applicable local authority area. There is ongoing debate and uncertainty within the U.K. as to how growing care needs will be met and funded in the future, and it is not clear at this stage what, if any, or the extent of such, impact will be on our U.K-based operators.
Additionally, there has been significant legislation passed and guidance issued in the U.K. in respect of the COVID-19 pandemic. Much of the legislation or guidance set out the additional precautions, measures or restrictions which were required in the care sector, including infection control measures and vaccination requirements for care sector workers. In addition, the U.K. government provided certain support to the care sector, including the provision of free testing and personal protective equipment (“PPE”) in certain settings. The U.K. government also provided some financial support to the sector, predominantly to publicly-funded services but also relation to infection control and testing measures it had introduced. This additional legislation has significantly increased the regulatory burdens under which our U.K. operators must currently deliver services and continues to have a significant impact on the operations and financial condition of our U.K. operators, which has been somewhat offset by the level of stimulus provided.
Environmental, Social and Governance ("ESG")
We prioritize environmental, social and governance initiatives that matter most to our business and shareholders. Our Nominating and Corporate Governance Committee of our Board of Directors has been charged with primary oversight of our sustainability efforts. The Company has established an ESG Steering Committee, with senior representation from all divisions of the company, that is responsible for advancing the Company’s governance, sustainability, and social programs, including diversity and inclusion. The Nominating and Corporate Governance Committee exercises oversight of the ESG Steering Committee.
As a triple-net landlord, our third-party operators maintain operational control and responsibility for our real estate on a day-to-day basis. While our ability to mandate environmental changes to their operations is limited, our tenants are contractually bound to preserve and maintain our properties in good working order and condition. In connection with this, they are required to meet or exceed annual expenditure thresholds on capital improvements and enhancements of our properties, which in some cases may facilitate improvements in the environmental performance of our properties and reduces energy usage, water usage, and direct and indirect greenhouse gas emissions. Beginning in 2021, we have also implemented a capital expenditure sustainability initiative to encourage operators to invest in financially beneficial and environmentally enhancing investment projects. The goal is to incentivize operators to invest in sustainable capital projects that provide a favorable return on investment while reducing the environmental footprint of these operations. Our due diligence on real estate acquisitions generally includes environmental assessments as part of our analysis to understand the environmental condition of the property, and to determine whether the property meets certain environmental standards. Similarly, during the due diligence process, we seek to evaluate the risk of physical, natural disaster or extreme weather patterns on the properties we are looking to acquire and to assess their compliance with building codes, which often results in remediations that incorporate sustainable improvements into our properties.
We are committed to providing a positive and engaging work environment for our employees and taking an active role in the betterment of the communities in which our employees live and work. See also "Human Capital Management" immediately below.
14
Additional information regarding our ESG programs and initiatives is available in the ESG section of our website at www.omegahealthcare.com. Information on our website, including our Corporate ESG Report or sections thereof, is not incorporated by reference into this Annual Report.
Human Capital Management
Our success is based on the focused passion and dedication of our people. We believe our employees’ commitment to Omega provides better service to our tenants and stakeholders, supports an inclusive and collegial working environment and generates long-term value for our shareholders and the communities which we serve. As of February 1, 2022, we had 70 employees including the executive officers listed below, none of whom is subject to a collective bargaining agreement. Due to the size and nature of our business, our future performance depends to a significant degree upon the continued contributions of our executive management team and other key employees. As such, the ability to attract, develop and retain qualified personnel will continue to be important to the Company’s long-term success.
We have a long-standing commitment to being an equal opportunity employer. In 2021, Omega was included in the Bloomberg Gender-Equality Index - one of only 380 companies worldwide, and fewer than 15 U.S. REITs, to be included in the 2021 index. In January 2022, Omega was included in the Bloomberg 2022 Gender-Equality Index for the third consecutive year. Additionally, in 2021, we reinforced our diversity and inclusion commitment by signing the CEO Action for Diversity and Inclusion Pledge, one of the largest CEO-driven business commitments to act on and advance diversity, equity and inclusion in the workplace. The Company has expanded its recruitment practices to reach more diverse candidates for employment and Board positions and has developed an internship program with a focus on increasing diversity in the pipeline of eligible employees. The Company requires employees and Board members to certify its Code of Business Conduct & Ethics periodically, and from time to time, conducts compliance training for all employees and Directors, including diversity and inclusion training. As of February 1, 2022, at the executive level, one of the Company’s four executive officers is a woman and brings ethnic diversity to the team, and on the senior management team, 25% are women and 25% bring ethnic diversity to the team.
We are committed to providing a positive and engaging work environment for our employees and taking an active role in the betterment of the communities in which our employees live and work. Our full-time employees are provided a competitive benefits program, including comprehensive healthcare benefits and a 401(k) plan with a matching contribution from the Company, the opportunity to participate in our employee stock purchase program, bonus and incentive pay opportunities, competitive paid time-off benefits and paid parental leave, wellness programs, continuing education and development opportunities, and periodic engagement surveys. In addition, we believe that giving back to our community is an extension of our mission to improve the lives of our stockholders, our employees, and their families. The Company has implemented a matching program for charitable contributions of employees.
Information about our Executive Officers
Biographical information regarding our executive officers and their ages as of February 1, 2022 are set forth below:
C. Taylor Pickett (60) is our Chief Executive Officer and has served in this capacity since June 2001. Mr. Pickett has also served as Director of the Company since May 30, 2002. Mr. Pickett has also been a member of the board of trustees of Corporate Office Properties Trust, an office REIT focusing on U.S. government agencies and defense contractors, since November 2013. From January 1993 to June 2001, Mr. Pickett served as a member of the senior management team of Integrated Health Services, Inc., most recently as Executive Vice President and Chief Financial Officer. Prior to joining Integrated Health Services, Inc. Mr. Pickett held various positions at PHH Corporation and KPMG Peat Marwick.
Daniel J. Booth (58) is our Chief Operating Officer and has served in this capacity since October 2001. From 1993 to October 2001, Mr. Booth served as a member of the management team of Integrated Health Services, Inc., most recently serving as Senior Vice President, Finance. Prior to joining Integrated Health Services, Inc., Mr. Booth served as a Vice President in the Healthcare Lending Division of Maryland National Bank (now Bank of America).
15
Robert O. Stephenson (58) is our Chief Financial Officer and has served in this capacity since August 2001. From 1996 to July 2001, Mr. Stephenson served as the Senior Vice President and Treasurer of Integrated Health Services, Inc. Prior to joining Integrated Health Services, Inc., Mr. Stephenson held various positions at CSX Intermodal, Inc., Martin Marietta Corporation and Electronic Data Systems.
Gail D. Makode (46) is our Chief Legal Officer, General Counsel and has served in this capacity since September 2019. Previously, she served as Senior Vice President, General Counsel and Corporate Secretary of IES Holdings, Inc., from October 2012 to September 2019. Prior to IES, she served in various legal capacities at MBIA Inc., including as General Counsel and Member of the Board at MBIA Insurance Corporation and Chief Compliance Officer of MBIA Inc., from 2006 to 2012. Earlier in her career, she served as Vice President and Counsel for Deutsche Bank AG, and as an associate at Cleary, Gottlieb, Steen, & Hamilton, where she specialized in public and private securities offerings and mergers and acquisitions.
Available Information
Our website address is www.omegahealthcare.com. Our Annual Reports on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and any amendments to those reports filed or furnished pursuant to Section 13(a) or 15(d) of the Securities Exchange Act of 1934 (the “Exchange Act”) are available on our website, free of charge, as soon as reasonably practicable after we electronically file such materials with, or furnish them to, the U.S. Securities and Exchange Commission (“SEC”). Additionally, the SEC maintains a website that contains reports, proxy and information statements, and other information regarding issuers that file electronically with the SEC, including us, at www.sec.gov.
Item 1A – Risk Factors
This section discusses material risk factors that may affect our business, operations and financial condition. It does not describe all risks and uncertainties applicable to us, our industry or ownership of our securities. If any of the following risks, or any other risks and uncertainties that are not addressed below or that we have not yet identified, actually occur, we could be materially adversely affected and the value of our securities could decline.
Risks Related to the Operators of Our Facilities
Our financial position could be weakened and our ability to make distributions and fulfill our obligations with respect to our indebtedness could be limited if our operators, or a portion thereof, become unable to meet their obligations to us or fail to renew or extend their relationship with us as their lease terms expire or their mortgages mature, or if we become unable to lease or re-lease our facilities or make mortgage loans on economically favorable terms. We have no operational control over our operators.
The bankruptcy or insolvency of our operators could limit or delay our ability to recover on our investments.
We are exposed to the risk that a distressed or insolvent operator may not be able to meet its lease, loan, mortgage or other obligations to us or other third parties. This risk is heightened during a period of economic or political instability. Although each of our lease and loan agreements typically provides us with the right to terminate, evict an operator, foreclose on our collateral, demand immediate payment and exercise other remedies upon the bankruptcy or insolvency of an operator, title 11 of the U.S. Code (the “Bankruptcy Code”) would limit or, at a minimum, delay our ability to collect unpaid pre-bankruptcy rents and mortgage payments and to pursue other remedies against a bankrupt operator. While we sometimes have third-party guarantees of an operator’s lease or loan obligations, such guarantees can be expensive to enforce, and have their own risks of collection as against the guarantors.
16
Leases. A bankruptcy filing by one of our lessee operators would typically prevent us from collecting unpaid pre-bankruptcy rents or evicting the operator, absent approval of the bankruptcy court. The Bankruptcy Code provides a lessee with the option to assume or reject an unexpired lease within certain specified periods of time. Generally, a lessee is required to pay all rent that becomes payable between the date of its bankruptcy filing and the date of the assumption or rejection of the lease (although such payments will likely be delayed as a result of the bankruptcy filing). If one of our lessee operators chooses to assume its lease with us, the operator must promptly cure all monetary defaults existing under the lease (including payment of unpaid pre-bankruptcy rents) and provide adequate assurance of its ability to perform its future lease obligations. Even where a lessee operator assumes its lease with us, it will first often threaten to reject that lease to obtain better lease terms from us, and we sometimes have to consider making, or we do make, such economic concessions to avoid rejection of the lease and our taking a closed facility back. If one of our lessee operators opts to reject its lease with us, we would have a claim against such operator for unpaid and future rents payable under the lease, but such claim would be subject to a statutory “cap” under the Bankruptcy Code, and would likely result in a recovery substantially less than the face value of such claim. Although the operator’s rejection of the lease would permit us to recover possession of the leased facility, we would likely face losses, costs and delays associated with repairs and/or maintenance of the facility and then re-leasing the facility to a new operator, or costs associated with selling the facility. In any event, re-leasing a facility or selling it could take a material amount of time, and the pool of interested and qualified tenants or buyers will be limited due to the unique nature of our properties, which may depress values and our eventual recovery. Finally, whether a lease operator in bankruptcy ends up assuming or rejecting our lease, we will incur legal and collection costs, which can be difficult or impossible to recover.
Several other factors could impact our rights under leases with bankrupt operators. First, the operator could seek to assign its lease with us to a third party. The Bankruptcy Code disregards anti-assignment provisions in leases to permit the assignment of unexpired leases to third parties (provided all monetary defaults under the lease are promptly cured and the assignee can demonstrate its ability to perform its obligations under the lease). Second, in instances in which we have entered into a master lease agreement with an operator that operates more than one facility, the bankruptcy court could determine that the master lease was comprised of separate, divisible leases (each of which could be separately assumed or rejected), rather than a single, integrated lease (which would have to be assumed or rejected in its entirety). Finally, the bankruptcy court could re-characterize our lease agreement as a disguised financing arrangement, which could require us to receive bankruptcy court approval to foreclose or pursue other remedies with respect to the facility.
Mortgages. A bankruptcy filing by an operator to which we have made a loan secured by a mortgage would typically prevent us from collecting unpaid pre-bankruptcy mortgage payments and foreclosing on our collateral, absent approval of the bankruptcy court. As an initial matter, we could ask the bankruptcy court to order the operator to make periodic payments or provide other financial assurances to us during the bankruptcy case (known as “adequate protection”), but the ultimate decision regarding “adequate protection” (including the timing and amount of any “adequate protection” payments) rests with the bankruptcy court. In addition, we would need bankruptcy court approval before commencing or continuing any foreclosure action against the operator’s collateral (including a facility). The bankruptcy court could withhold such approval, especially if the operator can demonstrate that the facility or other collateral is necessary for an effective reorganization and that we have a sufficient “equity cushion” in the facility or that we are otherwise protected from any diminution in value of the collateral. If the bankruptcy court does not either grant us “adequate protection” or permit us to foreclose on our collateral, we may not receive any loan payments until after the bankruptcy court confirms a plan of reorganization for the operator. In addition, in any bankruptcy case of an operator to which we have made a loan, the operator may seek bankruptcy court approval to pay us (i) over a longer period of time than the terms of our loan, (ii) at a different interest rate, and/or (iii) for only the value of the collateral, instead of the full amount of the loan. Finally, even if the bankruptcy court permits us to foreclose on the facility, we would still be subject to the losses, costs and other risks associated with a foreclosure sale, including possible successor liability under government programs, indemnification obligations and suspension or delay of third-party payments. Should such events occur, our income and cash flow from operations would be adversely affected.
17
Failure by our operators to comply with government regulations may adversely impact their ability to make debt or lease payments to us.
Our operators are subject to numerous federal, state and local laws and regulations in the U.S. and, for certain operators, in the U.K., including those described in Item 1. Business – Government Regulation and Reimbursement. Laws and regulations impacting our operators include, without limitation, those relating to reimbursement (including Medicare and Medicaid reimbursement programs in the US), quality of care initiatives, licensing and certification of our operators, fraud and abuse laws and regulations, privacy and security laws. Other federal, state and local laws and regulations also affect how our operators conduct their operations. We cannot predict the effect that the costs of complying with these laws may have on the revenues of our operators, and thus their ability to meet their obligations to us. In addition, requirements applicable to our operators are subject to frequent and substantial changes (sometimes applied retroactively) resulting from new legislation, adoption of rules and regulations, and administrative and judicial interpretations of existing law, and any changes in the regulatory framework could have a material adverse effect on our tenants, operators, guarantors and managers. Any of these changes may be more pronounced following federal and state leadership changes and particularly following a change in presidential administrations. The ultimate timing or effect of these changes cannot be predicted. These changes may have a dramatic effect on our operators’ costs of doing business and on the amount of reimbursement by both government and other third-party payors. The failure of any of our operators to comply with these laws, requirements and regulations could adversely affect their ability to meet their obligations to us. If we fail to effectively implement or appropriately adjust our operational and strategic initiatives with respect to the implementation of new laws and regulations, or do not do so as effectively as our competitors, our results of operations may be materially adversely affected.
Our U.S. operators depend on reimbursement from governmental and other third-party payors, and reimbursement rates from such payors may be reduced or modified, including through reductions to the Medicare and Medicaid programs.
Changes in the reimbursement rate or methods of payment from governmental and other third-party payors, including the Medicare and Medicaid programs, or the implementation of other measures to reduce reimbursements for services provided by our operators has in the past, and could in the future, result in a substantial reduction in our operators’ revenues and operating margins. Reimbursement from governmental and other third-party payors could be reduced as part of spending cuts and tax reform initiatives that impact Medicare, Medicaid or Medicare Advantage Plans, or as part of retroactive adjustments during claims settlement processes or as a result of post-payment audits. Further, alternative payment models, as well as other legislative initiatives, have the potential to affect Medicare payments to SNFs, including, but not limited to, provisions changing the payment methodology, setting reimbursement caps, implementing value based purchasing and payment bundling, and studying the appropriateness of restrictions on payments for healthcare acquired conditions. In some cases, states have enacted or are considering enacting measures designed to reduce Medicaid expenditures or freeze Medicaid rates and to make changes to private healthcare insurance, and several commercial payors have expressed an intent to pursue certain value-based purchasing models and initiatives. Since our operators’ profit margins on Medicaid patients are generally relatively low, more than modest reductions in Medicaid reimbursement and an increase in the number of Medicaid patients could place some operators in financial distress, which in turn could adversely affect us. If funding for Medicare and/or Medicaid is reduced, it could have a material adverse effect on our operators’ results of operations and financial condition, which could adversely affect our operators’ ability to meet their obligations to us. Significant limits on the scope of services reimbursed and on reimbursement rates, as well as changes in reimbursement policies or other measures altering payment methodologies for services provided by our operators, could have a material adverse effect on our operators’ results of operations and financial condition, which could cause the revenues of our operators to decline and negatively impact their ability to meet their obligations to us.
We may be unable to find a replacement operator for one or more of our leased properties.
From time to time, we need to find a replacement operator for one or more of our leased properties for a variety of reasons, including upon the expiration of the lease term or the occurrence of an operator default. While we are attempting to locate one or more replacement operators, we sometimes experience and may in the future experience a decrease or cessation of rental payments on the applicable property or properties. We cannot assure you that any of our current or future operators will elect to renew their respective leases with us upon expiration of the terms thereof. Similarly, we cannot assure you that we will be able to locate a suitable replacement operator or, if we are successful in locating a replacement operator, that the rental payments from the new operator would not be significantly less than the existing rental payments. Our ability to locate a suitable replacement operator may be significantly delayed or limited by various state licensing, receivership, certificate of need or other laws, as well as by Medicare and Medicaid change-of-ownership rules. We also may incur substantial additional expenses in connection with any such licensing, receivership or change-of-ownership proceedings. Any such delays, limitations and expenses could materially delay or impact our ability to collect rent, obtain possession of leased properties or otherwise exercise remedies for default.
18
Our operators may be subject to significant legal actions that could result in their increased operating costs and substantial uninsured liabilities, which may affect their ability to meet their obligations to us; and we may become party to such legal actions.
Our operators may be subject to claims for damages relating to the services that they provide. While we are unable to predict the scope of future federal, state and local regulations and legislation, including the Medicare and Medicaid statutes and regulations, we believe that long-term care providers will continue to be the focus of governmental investigations, particularly in the area of Medicare/Medicaid false claims and in the use of COVID-19 related funds and compliance with infection control and quality standards. We can give no assurance that the insurance coverage maintained by our operators will cover all claims made against them or continue to be available at a reasonable cost, if at all. In some states, insurance coverage for the risk of punitive damages arising from professional and general liability claims and/or litigation may not, in certain cases, be available to operators due to state law prohibitions or limitations of availability. As a result, our operators operating in these states may be liable for punitive damage awards that are either not covered or are in excess of their insurance policy limits.
Any adverse determination in a legal proceeding or governmental investigation, whether currently asserted or arising in the future, could have a material adverse effect on an operator’s financial condition and its ability to meet its obligations to us, which, in turn, could have a material adverse effect on our business, financial condition, results of operations and ability to make distributions to our stockholders.
In addition, we may in some circumstances be named as a defendant in litigation involving the services provided by our operators. In the past, we and several of our wholly-owned subsidiaries have been named as defendants in professional liability and general liability claims related to our owned and operated facilities, and we could be named as defendants in similar suits in the future. In these suits, patients of our operators have alleged significant damages, including punitive damages, against the defendants. Although we generally have no involvement in the services provided by our operators, and our standard lease and loan agreements generally require our operators to indemnify us and carry insurance to cover us in certain cases, a significant judgment against us in such litigation could exceed our and our operators’ insurance coverage, which would require us to make payments to cover the judgment.
Increased competition as well as increased operating costs result in lower revenues for some of our operators and may affect the ability of our operators to meet their obligations to us.
The long-term healthcare industry is highly competitive and we expect that it may become more competitive in the future. Our operators are competing with numerous other companies providing similar healthcare services or alternatives such as home health agencies, life care at home, community-based service programs, retirement communities and convalescent centers. Our operators compete on a number of different levels including the quality of care provided, reputation, the physical appearance of a facility, price, the range of services offered, family preference, alternatives for healthcare delivery, the supply of competing properties, physicians, staff, referral sources, location and the size and demographics of the population in the surrounding areas. Our operators may encounter increased competition in the future that could limit their ability to attract residents or expand their businesses and therefore affect their ability to pay their lease or mortgage payments and meet their obligations to us.
In addition, the market for qualified personnel is highly competitive and our operators may experience difficulties in attracting and retaining such personnel, in particular due to labor constraints and, in some cases, wage increases imposed by the COVID-19 pandemic. Increases in labor costs could affect our operators’ ability to meet their obligations to us, which could be particularly acute in certain states that have established minimum staffing requirements.
We may be unable to successfully foreclose on the collateral securing our mortgage loans, and even if we are successful in our foreclosure efforts, we may be unable to successfully find a replacement operator, or operate or occupy the underlying real estate, which may adversely affect our ability to recover our investments.
If an operator defaults under one of our mortgage loans, we may foreclose on the loan or otherwise protect our interest by acquiring title to the property. In such a scenario, we may be required to make substantial improvements or repairs to maximize the facility’s investment potential. Operators may contest enforcement of foreclosure or other remedies, seek bankruptcy protection against our exercise of enforcement or other remedies and/or bring claims for lender liability in response to actions to enforce mortgage obligations. Even if we are able to successfully foreclose on the collateral securing our mortgage loans, we may be unable to expeditiously find a replacement operator, if at all, or otherwise successfully operate or occupy the property, which could adversely affect our ability to recover our investment.
19
Uninsured losses or losses in excess of our operators’ insurance coverage could adversely affect our financial position and our cash flow.
Under the terms of our leases, our operators are generally required to maintain comprehensive general liability, fire, flood, earthquake, boiler and machinery, nursing home or long-term care professional liability and extended coverage insurance with respect to our properties with policy specifications set forth in the leases or other written agreements between us and the operator. However, our properties may be adversely affected by casualty losses which exceed insurance coverages and reserves. In addition, we cannot provide any assurances that our tenants will maintain the required coverages, that we will continue to require the same levels of insurance under our leases, or that such insurance will be available at a reasonable cost in the future or that the policies maintained will fully cover all losses on our properties upon the occurrence of a catastrophic event. We also cannot make any guaranty as to the future financial viability of the insurers that underwrite the policies maintained by our tenants, or, alternatively if our tenants utilize captive or self-insurance programs, that such programs will be adequately funded.
Should an uninsured loss or a loss in excess of insured limits occur, we could lose both our investment in, and anticipated profits and cash flows from, the property and disputes over insurance claims could arise. Even if it were practicable to restore the property to its condition prior to the damage caused by a major casualty, the operations of the affected property would likely be suspended for a considerable period of time.
Our development and redevelopment projects may not yield anticipated returns.
We consider and, when appropriate, invest in various development and redevelopment projects. In deciding whether to make an investment in a particular project, we make certain assumptions regarding the expected future performance of the property. Our assumptions are subject to risks generally associated with development and redevelopment projects, including, among others, that:
| ● | Our operators may not be able to complete the project on schedule or within budgeted amounts; |
| ● | Our operators may encounter delays in obtaining or fail to obtain all necessary zoning, land use, building, occupancy, environmental and other governmental permits and authorizations, or underestimate the costs necessary to develop or redevelop the property to market standards; |
| ● | Volatility in the price of construction materials or labor may increase project costs; |
| ● | The builders may fail to perform or satisfy the expectations of our operators; |
| ● | We may incorrectly forecast risks associated with development in new geographic regions; |
| ● | Demand for our project may decrease prior to completion, due to competition from other developments; and |
| ● | New facilities may take longer than expected to reach stabilized operating levels, if at all. |
If any of the risks described above occur, our development and redevelopment projects may not yield anticipated returns, which could have a material adverse effect on us.
Risks Related to Us and Our Operations
The COVID-19 pandemic and measures intended to prevent its spread could have a material adverse effect on our business, results of operations, cash flows and financial condition.
The COVID-19 pandemic has significantly and adversely impacted, and may continue to impact SNFs and long-term care providers due to higher rates of virus transmission and fatality among the elderly and frail populations these facilities serve. As a result, many of our operators have been, and may continue to be, significantly impacted by the pandemic. See Item 2 – Management’s Discussion and Analysis of Financial Condition and Results of Operations – Overview. During 2021, four of our operators have either missed contractual payments for a period or have informed us that they would be unable to pay us rent for the foreseeable future. We also placed six operators, including three of the non-paying operators, on a cash basis of revenue recognition during 2021, as collection of substantially all contractual lease payments with these six operators was no longer probable. We believe these operators were impacted by, among other things, reduced revenue as a result of lower occupancy and increased expenses resulting from the COVID-19 pandemic, as well as uncertainties regarding the availability of sufficient government support. In connection with these developments, we have written off approximately $36.0 million in aggregate of straight-line receivables to rental income for the year ended December 31, 2021 (in connection with the six operators placed on a cash basis during the year). We have also taken impairments of $83.4 million for the year ended December 31, 2021 in connection with loans outstanding with Agemo Holdings, LLC, Gulf Coast Health Care LLC and Guardian Healthcare, all of whom are non-paying operators. The six operators that were placed on a cash basis of revenue recognition in 2021 collectively represent 6.6% and 7.3% of our total revenue, respectively, for the year ended December 31, 2021 and 2020 (excluding the impact of write-offs in 2021 and 2020).
20
Continued uncertainty exists relating to our other operators’ ability to meet their payments obligations generally or meet their payment obligations to us, including due to continued uncertainty regarding the availability of sufficient government support, the persistence of staffing shortages that have impacted, and may continue to impact, our operators’ occupancy levels and profitability, the impact of governmental vaccine mandates for staff on ongoing staffing shortages, and other factors that may impact virus transmission in our facilities, including the impact of genetic mutations of the virus into new variants, as well as the commencement in April 2021 for many of our operators of the repayment of accelerated payments of Medicare funds that were previously received as Advanced Medicare payments in 2020, and the commencement in December 2021 of repayment of deferred FICA obligations. To the extent our operators are unable to meet their payment obligations, we may record additional impairment charges with respect to straight-line rent receivables associated with any such operator or with respect to outstanding loans and our financial condition could be adversely impacted. See “Our assets, including our real estate and loans, are subject to impairment charges, and our valuation and reserve estimates are based on assumptions and may be subject to adjustment” in Item 1A contained in Part I of this Annual Report on Form 10-K.
Our operators have been, and continue to be, impacted by the pandemic in numerous ways. In addition to experiencing outbreaks of positive cases and deaths of residents and employees during the pandemic, our operators have been required to, and continue to, adapt their operations rapidly throughout the pandemic to manage the spread of the COVID-19 virus as well as the implementation of new treatments and vaccines, and to implement new requirements relating to infection control, staffing levels, PPE, quality of care, visitation protocols, and reporting, among other regulations, throughout the pandemic while facing staffing shortages that have accelerated during the pandemic and that may impede the delivery of care. The federal government announced in August and September 2021 that it would be requiring SNF and healthcare workers to be vaccinated against COVID-19 and has issued an emergency implementing regulation effective November 5, 2021 requiring covered healthcare facilities to ensure eligible staff have received a first vaccine dose as of December 5, 2021 and a second dose of a two-dose vaccine as of January 4, 2022, with certain permitted exemptions in alignment with federal law; these vaccination deadlines were subsequently extended by CMS by between one to two months depending on the applicable state. Significant uncertainty remains regarding the potential impact such mandates may have on ongoing staffing shortages in our facilities, which have caused some operators to limit admissions. In addition, it remains uncertain when and to what extent vaccination programs for COVID-19, which have been implemented in most of our facilities, will continue to mitigate the effects of COVID-19 in our facilities, or how effective existing vaccines and booster doses will be against the variants of the COVID-19 virus; the impact of these programs will depend in part on the continued speed, distribution, efficacy and delivery of the vaccine and booster doses in our facilities, compliance with staff vaccination requirements as well as participation levels in vaccination programs among the residents and employees of our operators. Our operators have continued to report considerable variation in participation levels among both employees and residents, which we believe may change over time with additional vaccination education efforts for residents and implementation of vaccine mandates for staff.
In addition to the risks associated with managing the spread of the virus, delivery of the vaccines and care of their patients and residents, many of our operators reported incurring, and may continue to incur, significant cost increases as a result of the COVID-19 pandemic, with dramatic increases for facilities with positive cases. We believe these increases primarily stem from elevated labor costs, in part as a result of staffing shortages, including the increased use of overtime and bonus pay and reliance on agency staffing, as well as a significant increase in both the cost and usage of PPE, testing equipment and processes and supplies, as well as implementation of new infection control protocols and delivery of the vaccine. In addition, many of our operators have experienced declines in occupancy levels as a result of the pandemic. We believe these declines may be in part due to staffing shortages, which in some cases have required operators to limit admissions, as well as COVID-19-induced fatalities at the facilities, the delay of SNF placement and/or utilization of alternative care settings for those with lower level of care needs, the suspension or postponement of elective hospital procedures, fewer discharges from hospitals to SNFs and higher hospital readmittances from SNFs. We continue to monitor the impact of occupancy levels at many of our operators, and it remains uncertain whether and when demand and occupancy levels will return to pre-COVID-19 levels.
21
Federal relief efforts for SNFs and ALFs was limited in 2021 as have been relief efforts in certain states, and further government support will likely be needed to continue to offset these impacts. It is unclear whether and to what extent such government support has been and will continue to be sufficient and timely to offset these impacts. In particular, it remains unclear whether relief will be distributed to our operators in any meaningful way or whether additional Medicaid funds will ultimately support reimbursement to our operators. Further, to the extent the impacts of the pandemic continue or accelerate and are not offset by continued government relief that is sufficient and timely, we anticipate that the operating results of certain of our operators would be materially and adversely affected, some may be unwilling or unable to pay their contractual obligations to us in full or on a timely basis and we may be unable to restructure such obligations on terms as favorable to us as those currently in place. Even if operators are able to avail themselves of government relief to offset some of these costs, they may face challenges in complying with the terms and conditions of government support and may face longer-term adverse impacts to their personnel and business operations from the COVID-19 pandemic, including potential patient litigation and decreased demand for their services, loss of business due to an interruption in their operations, workforce challenges, new regulatory restrictions, or other liabilities related to gathering restrictions, quarantines, reopening plans, vaccine distribution or delivery, spread of infection or other related factors.
Numerous state and local governments and the federal government have initiated efforts that may also affect landlords’ and/or mortgagees’ ability to collect payments due or enforce remedies for the failure to pay amounts due. Additionally, a number of professional liability and employment related claims have been filed or are threatened to be filed against long-term care providers related to the COVID-19 pandemic. While such claims may be subject to liability protection provisions within various state executive orders or legislation and/or federal legislation, an adverse resolution of any of legal proceeding or investigations against our operators may involve injunctive relief and/or substantial monetary penalties, either or both of which could have a material adverse effect on our reputation, business, results of operations and cash flows.
The COVID-19 pandemic has from time to time also caused, and may continue to cause, severe economic, market and other disruptions worldwide. The pandemic has led governments and other authorities in the U.S., U.K. and around the world to impose measures intended to control its spread, including but not limited to, restrictions on freedom of movement and business operations which may remain in place or be reinstated along with continuing uncertainty around the potential duration of the pandemic. We cannot assure you that conditions in the bank lending, capital and other financial markets will not deteriorate or fluctuate as a result of the COVID-19 pandemic, or that our access to capital and other sources of funding will not become constrained, which could adversely affect the availability and terms of future borrowings, renewals or refinancing. In addition, our employees may be impacted directly or indirectly by the pandemic and we may be required to make changes to our internal controls as a result of changes in our business processes or personnel; any such changes may increase our operational and financial reporting risks.
The extent of the COVID-19 pandemic’s effect on our and our operators’ operational and financial performance will depend on future developments, including the ability to control the spread of the outbreak generally and in our facilities, and the delivery and efficacy of and participation in vaccination programs and other treatments for COVID-19, government funds and other support for the senior care sector and the efficacy of other policies and measures that may mitigate the impact of the pandemic, as well as the future demand for needs-based skilled nursing care and senior living facilities, all of which are uncertain and difficult to predict. Due to these uncertainties, we are not able at this time to estimate the effect of these factors on our business, but the adverse impact on our business, results of operations, financial condition and cash flows could be material.
There are no assurances of our ability to pay dividends in the future.
Our ability to pay dividends may be adversely affected upon the occurrence of any of the risks described herein. Our payment of dividends is subject to compliance with restrictions contained in our credit agreements, the indentures governing our senior notes and any preferred stock that our Board may from time to time designate and authorize for issuance. All dividends will be paid at the discretion of our Board and will depend upon our earnings, our financial condition, maintenance of our REIT status and such other factors as our Board may deem relevant from time to time. There are no assurances of our ability to pay dividends in the future. In addition, our dividends in the past have included, and may in the future include a return of capital.
22
We rely on external sources of capital to fund future capital needs, and if we encounter difficulty in obtaining such capital, we may not be able to make future investments necessary to grow our business or meet maturing commitments.
As a REIT under the Code, we are required to, among other things, distribute at least 90% of our REIT taxable income each year to our stockholders. Because of this distribution requirement, we may not be able to fund, from cash retained from operations, all future capital needs, including capital needed to make investments and to satisfy or refinance maturing commitments. As a result, we rely on external sources of capital, including debt and equity financing. If we are unable to obtain needed capital at all or only on unfavorable terms from these sources, we might not be able to make the investments needed to grow our business, or to meet our obligations and commitments as they mature, which could negatively affect the ratings of our debt and even, in extreme circumstances, affect our ability to continue operations. We may not be in a position to take advantage of future investment opportunities in the event that we are unable to access the capital markets on a timely basis or we are only able to obtain financing on unfavorable terms.
Our ability to raise capital through equity sales is dependent, in part, on the market price of our common stock, and our failure to meet market expectations with respect to our business, or other factors we do not control, could negatively impact such market price and availability of equity capital.
As with other publicly-traded companies, the availability of equity capital will depend, in part, on the market price of our common stock which, in turn, will depend upon various market conditions and other factors, some of which we cannot control, that may change from time to time including:
| ● | the extent of investor interest; |
| ● | the general reputation of REITs and the attractiveness of their equity securities in comparison to other equity securities, including securities issued by other real estate-based companies; |
| ● | the financial performance of us and our operators; |
| ● | concentrations in our investment portfolio by tenant and facility type; |
| ● | concerns about our tenants’ financial condition due to uncertainty regarding reimbursement from governmental and other third-party payor programs; |
| ● | our credit ratings and analyst reports on us and the REIT industry in general, including recommendations, and our ability to meet our guidance estimates or analysts’ estimates; |
| ● | general economic, global and market conditions, including changes in interest rates on fixed income securities, which may lead prospective purchasers of our common stock to demand a higher annual yield from future distributions; |
| ● | our failure to maintain or increase our dividend, which is dependent, to a large part, on the increase in funds from operations, which in turn depends upon increased revenues from additional investments and rental increases; and |
| ● | other factors such as governmental regulatory action and changes in REIT tax laws, as well as changes in litigation and regulatory proceedings. |
The market value of the equity securities of a REIT is generally based upon the market’s perception of the REIT’s growth potential and its current and potential future earnings and cash distributions. Our failure to meet the market’s expectation with regard to future earnings and cash distributions would likely adversely affect the market price of our common stock and, as a result, the availability of equity capital to us.
We are subject to risks associated with debt financing, including changes in our credit ratings, which could negatively impact our business and limit our ability to make distributions to our stockholders and to repay maturing debt.
The financing required to make future investments and satisfy maturing commitments may be provided by borrowings under our credit facilities, private or public offerings of debt or equity, the assumption of secured indebtedness, mortgage financing on a portion of our owned portfolio or through joint ventures. To the extent we must obtain debt financing from external sources to fund our capital requirements, we cannot guarantee such financing will be available on favorable terms, if at all. In addition, if we are unable to refinance or extend principal payments due at maturity or pay them with proceeds from other capital transactions, our cash flow may not be sufficient to make distributions to our stockholders and repay our maturing debt. Furthermore, if prevailing interest rates, changes in our debt credit ratings or other factors at the time of refinancing result in higher interest rates upon refinancing, the interest expense relating to that refinanced indebtedness would increase, which could reduce our profitability and the amount of dividends we are able to pay. Factors that may affect our credit ratings include, among other things, our financial performance, our success in raising sufficient equity capital, adverse changes in our debt and fixed charge coverage ratios, our capital structure and level of indebtedness and pending or future changes in the regulatory framework applicable to our operators and our industry. Further, additional debt financing increases the amount of our leverage. The degree of leverage could have important consequences to stockholders, including affecting our investment grade ratings and our ability to obtain additional financing in the future, and making us more vulnerable to a downturn in our results of operations or the economy generally.
23
The interest rate of our credit facilities, term loan facilities and derivatives contracts are priced using LIBOR and are subject to risks associated with the transition from LIBOR to an alternative reference rate.
London Inter-bank Offered Rate (“LIBOR”) is the basic rate of interest used in lending between banks on the London interbank market and is widely used as a reference for setting the interest rate on loans globally. We typically use LIBOR as a reference rate in credit facilities, term loan facilities and derivative contracts. In July 2017, the U.K.’s Financial Conduct Authority (“FCA”) that regulates LIBOR announced that it intends to stop compelling banks to submit rates for the calculation of LIBOR after 2021, and while the transition period for many LIBOR tenors has been extended to June 2023, the U.S. Federal Reserve advised banks to stop new LIBOR issuances by the end of 2021. At this time, no consensus exists as to which reference rate or rates or benchmarks may become acceptable alternatives to LIBOR. The Alternative Reference Rates Committee, a steering committee comprised of U.S. financial market participants, has identified the secured overnight financing rate, or SOFR, as the recommended alternative rate for all LIBOR. At this time, it is impossible to predict whether the SOFR or another reference rate will become an accepted alternative to LIBOR. Any changes in the methods by which LIBOR is determined or regulatory activity related to LIBOR’s phaseout could cause LIBOR to perform differently than in the past or cease to exist. Further, the consequences of these developments, or any alternative reference rate that is adopted, cannot be entirely predicted but could include an increase in the cost of our variable rate borrowings, of which we had $50 million of borrowings outstanding as of December 31, 2021 and $450 million notional value derivative instruments that are indexed to LIBOR. For some instruments, the method of transitioning to an alternative rate may be challenging, as this may require negotiation with the respective counterparty.
We may be subject to additional risks in connection with our acquisitions of long-term care facilities.
We may be subject to additional risks in connection with our acquisitions of long-term care facilities, including but not limited to the following:
| ● | our limited prior business experience with certain of the operators of the facilities we have recently acquired or may acquire in the future; |
| ● | the facilities may underperform due to various factors, including unfavorable terms and conditions of the lease agreements that we assume, disruptions caused by the management of the operators of the facilities or changes in economic conditions impacting the facilities and/or the operators; |
| ● | large acquisitions or investments could place significant additional demands on, and require us to expand, our management, resources and personnel, as well as to adapt our administrative, accounting and operational systems to integrate and manage the long-term care facilities we have acquired or may acquire in a timely manner; |
| ● | diversion of our management’s attention away from other business concerns; |
| ● | exposure to any undisclosed or unknown potential liabilities relating to the facilities; and |
| ● | potential underinsured losses on the facilities. |
We cannot assure you that we will be able to manage our recently acquired facilities, or the future growth in our business, without encountering difficulties or that any such difficulties will not have a material adverse effect on us. Our growth could also increase our capital requirements, which may require us to issue potentially dilutive equity securities and incur additional debt.
Our assets, including our real estate and loans, are subject to impairment charges, and our valuation and reserve estimates are based on assumptions and may be subject to adjustment.
Our asset portfolio primarily consists of real estate and mortgage loans, which are subject to write-downs in value. From time to time, we close facilities and actively market such facilities for sale. To the extent we are unable to sell these properties for our book value, we may be required to take a non-cash impairment charge or loss on the sale, either of which would reduce our net income. In addition, we periodically, but not less than annually, evaluate our real estate investments and other assets for impairment indicators, and we establish general and specific reserves for our issued loans at least quarterly. The quarterly evaluation of our investments for impairment may result in significant fluctuations in our provision for credit losses or real estate impairments from quarter to quarter, impacting our results of operations. Judgments regarding the existence of impairment indicators or loan reserves are based on a number of factors, including market conditions, operator performance and legal structure, and these factors may involve estimates. If we determine that a significant impairment has occurred, we are required to make an adjustment to the net carrying value of the asset, which could have a material adverse effect on our results of operations. Our estimates of loan reserves, and other accounting estimates, are inherently uncertain and may be subject to future adjustment, leading potentially to an increase in reserves.
24
Our indebtedness could adversely affect our financial condition.
We have a material amount of indebtedness and we may increase our indebtedness in the future. Our level and type of indebtedness could have important consequences for our stockholders. For example, it could:
| ● | increase our vulnerability to adverse changes in general economic, industry and competitive conditions; |
| ● | limit our ability to borrow additional funds, on satisfactory terms or at all, for working capital, capital expenditures, acquisitions, debt service requirements, execution of our business plan or other general corporate purposes; |
| ● | increase our cost of borrowing; |
| ● | require us to dedicate a substantial portion of our cash flow from operations to make payments on our indebtedness, thereby reducing the availability of our cash flow to fund working capital, capital expenditures and other general corporate purposes; |
| ● | limit our ability to make material acquisitions or take advantage of business opportunities that may arise; |
| ● | limit our ability to make distributions to our stockholders, which may cause us to lose our qualification as a REIT under the Code or to become subject to federal corporate income tax on any REIT taxable income that we do not distribute; |
| ● | expose us to fluctuations in interest rates, to the extent our borrowings bear variable rates of interest; |
| ● | limit our flexibility in planning for, or reacting to, changes in our business and the industry in which we operate; and |
| ● | place us at a competitive disadvantage compared to our competitors that have less debt. |
Further, we have the ability to incur substantial additional debt, including secured debt, which could intensify the risks above. In addition, if we are unable to refinance any of our floating rate debt, we would continue to be subject to interest rate risk. The short-term nature of some of our debt also subjects us to the risk that market conditions may be unfavorable or may prevent us from refinancing our debt at or prior to their existing maturities. In addition, our cash flow from operations may not be sufficient to repay all of our outstanding debt as it becomes due, and we may not be able to borrow money, sell assets or otherwise raise funds on acceptable terms, if at all, to refinance our debt.
Covenants in our debt documents limit our operational flexibility, and a covenant breach could materially adversely affect our operations.
The terms of our credit agreements and note indentures require us to comply with a number of customary financial and other covenants that may limit our management’s discretion by restricting our ability to, among other things, incur additional debt, redeem our capital stock, enter into certain transactions with affiliates, pay dividends and make other distributions, make investments and other restricted payments, engage in mergers and consolidations, create liens, sell assets or engage in new lines of business. In addition, our credit facilities require us to maintain compliance with specified financial covenants, including those relating to maximum total leverage, maximum secured leverage, maximum unsecured leverage, minimum fixed charge coverage, minimum consolidated tangible net worth and minimum unsecured interest coverage. Any additional financing we may obtain could contain similar or more restrictive covenants. Our continued ability to incur indebtedness, conduct our operations, and take advantage of business opportunities as they arise is subject to compliance with these financial and other covenants. Breaches of these covenants could result in defaults under the instruments governing the applicable indebtedness, in addition to any other indebtedness cross-defaulted against such instruments. Any such breach could materially adversely affect our business, results of operations and financial condition.
We are subject to particular risks associated with real estate ownership, which could result in unanticipated losses or expenses.
Our business is subject to many risks that are associated with the ownership of real estate. For example, if our operators do not renew their leases, we may be unable to re-lease the facilities at favorable rental rates, if at all. Other risks that are associated with real estate acquisition and ownership include, without limitation, the following:
| ● | general liability, property and casualty losses, some of which may be uninsured; |
| ● | the inability to purchase or sell our assets rapidly to respond to changing economic conditions, due to the illiquid nature of real estate and the real estate market; |
| ● | leases that are not renewed or are renewed at lower rental amounts at expiration; |
| ● | contingent rent escalators tied to changes in the Consumer Price Index or other parameters; |
| ● | the exercise of purchase options by operators resulting in a reduction of our rental revenue; |
| ● | costs relating to maintenance and repair of our facilities and the need to make expenditures due to changes in governmental regulations, including the Americans with Disabilities Act; |
| ● | environmental hazards created by prior owners or occupants, existing tenants, mortgagors or other persons for which we may be liable; and |
25
| ● | acts of God or terrorism affecting our properties. |
Our real estate investments are relatively illiquid.
Real estate investments are relatively illiquid and generally cannot be sold quickly. The real estate market is affected by many factors which are beyond our control, including general economic conditions, availability of financing, interest rates and supply and demand. Additional factors that are specific to our industry also tend to limit our ability to vary our portfolio promptly in response to changes in economic or other conditions. For example, all of our properties are ‘‘special purpose’’ properties that cannot be readily converted into general residential, retail or office use. In addition, transfers of operations of nursing homes and other healthcare-related facilities are subject to extensive regulatory approvals. We cannot predict whether we will be able to sell any property for the price or on the terms set by us or whether any price or other terms offered by a prospective purchaser would be acceptable to us. We also cannot predict the length of time needed to find a willing purchaser and to close the sale of a property, or that we will have funds available to make necessary repairs and improvements to a property held for sale. To the extent we are unable to sell any properties for our book value, we may be required to take a non-cash impairment charge or loss on the sale, either of which would reduce our net income.
We face possible risks and costs associated with severe weather conditions, natural disasters or the physical effects of climate change.
A large number of our properties are located in areas particularly susceptible to revenue loss, cost increase or damage caused by severe weather conditions or natural disasters such as hurricanes, earthquakes, tornadoes, fires and floods, as well as the effects of climate change. To the extent that climate change impacts changes in weather patterns, our markets could experience more frequent and severe natural disasters. Operationally, such events could cause a major power outage, leading to a disruption of our operators’ operations or require them to incur additional cost associated with evacuation plans. Over time, any of these conditions could result in increased operator costs, delays in construction, resulting in increased construction costs, or in the inability of our operators to operate our facilities at all. Climate change and severe weather may also have indirect effects on our business by increasing the cost to our operators of, or decreasing the availability to our operators of, property insurance on terms they find acceptable, and by increasing the cost of energy, maintenance, repair of water and/or wind damage, and snow removal at our properties. In the event of a loss in excess of insured limits, we could lose our incremental capital invested in the affected property.
Although Congress has not yet enacted comprehensive federal legislation to address climate change, numerous states and municipalities have adopted laws and policies on climate change and emission reduction targets. Changes in federal, state and local legislation and regulation based on concerns about climate change could result in increased capital expenditures on our existing properties and our new development properties (for example, to improve their energy efficiency and/or resistance to severe weather) without a corresponding increase in revenue, resulting in adverse impacts to our net income. There can be no assurance that climate change and severe weather will not have a material adverse effect on our properties, operations, or business.
As an owner or lender with respect to real property, we may be exposed to possible environmental liabilities.
Under various federal, state and local environmental laws, ordinances and regulations, a current or previous owner of real property or a secured lender may be liable in certain circumstances for the costs of investigation, removal or remediation of certain hazardous or toxic substances at such property, as well as certain other potential related costs, including government fines and damages for injuries to persons and adjacent property. Such laws often impose liability without regard to whether the owner knew of, or was responsible for, the presence or disposal of such substances. As a result, liability may be imposed on the owner in connection with the activities of an operator of the property, and the owner’s liability could exceed the value of the property and/or the assets of the owner. In addition, the presence of such substances, or the failure to properly dispose of or remediate such substances, may adversely affect an operators’ ability to attract additional residents and our ability to sell or rent such property or to borrow using such property as collateral which, in turn, could negatively impact our revenues.
Although our leases and mortgage loans generally require the lessee and the mortgagor to indemnify us for certain environmental liabilities, they may be unable to fulfill their indemnification obligations to us, and the scope of such obligations may be limited. For instance, most of our leases do not require the lessee to indemnify us for environmental liabilities arising before the lessee took possession of the premises.
26
The industry in which we operate is highly competitive. Increasing investor interest in our sector and consolidation at the operator level or REIT level could increase competition and reduce our profitability.
Our business is highly competitive and we expect that it may become more competitive in the future. We compete for healthcare facility investments with other healthcare investors, including other REITs, some of which have greater resources and lower costs of capital than we do. Increased competition makes it more challenging for us to identify and successfully capitalize on opportunities that meet our business goals. If we cannot capitalize on our development pipeline, identify and purchase a sufficient quantity of healthcare facilities at favorable prices, or are unable to finance such acquisitions on commercially favorable terms, our business, results of operations and financial condition may be materially adversely affected. In addition, if our cost of capital should increase relative to the cost of capital of our competitors, the spread that we realize on our investments may decline if competitive pressures limit or prevent us from charging higher lease or mortgage rates.
Our charter and bylaws contain significant anti-takeover provisions which could delay, defer or prevent a change in control or other transactions that could provide our stockholders with the opportunity to realize a premium over the then-prevailing market price of our common stock.
Our charter and bylaws contain various procedural and other requirements which could make it difficult for stockholders to effect certain corporate actions. Our Board of Directors (“Board”) has the authority to issue additional shares of preferred stock and to fix the preferences, rights and limitations of the preferred stock without stockholder approval. In addition, our charter contains limitations on the ownership of our capital stock intended to ensure we continue to meet the requirements for qualification as a REIT. For example, our charter, among other restrictions, prohibits the beneficial or constructive ownership (as defined for federal income tax purposes) by any person of more than 9.8% in value or in number of shares of the outstanding shares of any class or series of our capital stock, unless our Board grants an exemption or modifies the ownership limit for such person and certain conditions are satisfied. These provisions could discourage unsolicited acquisition proposals or make it more difficult for a third party to gain control of us, which could adversely affect the market price of our securities and/or result in the delay, deferral or prevention of a change in control or other transactions that could provide our stockholders with the opportunity to realize a premium over the then-prevailing market price of our common stock.
Ownership of property outside the U.S. may subject us to different or greater risks than those associated with our U.S. investments, including currency fluctuations.
We have investments in the U.K., and may from time to time may seek to acquire other properties in the U.K. or otherwise outside the U.S. Although we currently have investments in the U.K., we have limited experience investing in healthcare properties or other real estate-related assets located outside the U.S. International development, investment, ownership and operating activities involve risks that are different from those we face with respect to our U.S. properties and operations. These risks include, but are not limited to, any international currency gain recognized with respect to changes in exchange rates may not qualify under the income tests that we must satisfy annually in order to qualify and maintain our status as a REIT; fluctuations in the exchange rates between USD and the British Pound Sterling (“GBP”), or other foreign currencies in which we may transact in the future, which we may be unable to protect against through hedging; changes in foreign political, regulatory, and economic conditions; challenges in managing international operations; challenges of complying with a variety of foreign laws and regulations, including those relating to real estate, healthcare operations, taxes, employment and legal proceedings; differences in lending practices and the willingness of domestic or foreign lenders to provide financing; regional or country-specific business cycles and economic instability; and changes in applicable laws and regulations in the U.S. that affect foreign operations. In addition, we have limited investing experience in international markets. If we are unable to successfully manage the risks associated with international expansion and operations, our results of operations and financial condition may be adversely affected.
On January 31, 2020, the U.K. withdrew from the European Union (“E.U.”), commonly referred to as “Brexit”. Changes in economic conditions in the U.K. relating to Brexit may subject the operators of our facilities in the U.K. to increased risk, including potential disruptions in supply, increases in costs, or difficulty staffing. In addition, the uncertainty related to Brexit has caused foreign exchange rate fluctuations in the past, including the strengthening of the USD relative to the Euro and GBP immediately following the announcement of Brexit, and may continue to do so in the future. Furthermore, Brexit could lead to legal uncertainty or the imposition of additional legal or regulatory requirements on the Company, which could have adverse consequences on our business, financial condition and results of operations. The implementation of, or further developments with respect to, Brexit could further impact foreign exchange rates, which could materially adversely affect our business, financial condition and results of operations. To date, one of the key effects of Brexit on the U.K. market is increased difficulty recruiting suitably qualified staff members within properties, as historically the E.U. and freedom of movement provided a reliable personnel resource for the U.K. market. The employment pool within the U.K. is further impacted by vaccination requirements for those working in the sector, meaning that those in certain roles who refuse to be vaccinated may not be employed (unless exempt from the requirement).
27
Our assets are concentrated in the long-term care industry and face geographic and operator concentration risk.
Our assets are generally not diversified by industry and face risks associated with the long-term care industry. In addition, at December 31, 2021, two operators each represented greater than 10% of our investments, and the three states in which we had our highest concentration of investments were Florida (15%), Texas (10%) and Michigan (6%). As a result, we are subject to increased exposure to adverse conditions affecting these operators and regions, with regional risks including unfavorable Medicaid reimbursements rates for SNFs, downturns in the local economies, local real estate conditions, increased competition or decreased demand for our facilities, regional climate events, and unfavorable legislative or regulatory developments, which could adversely affect our business and results of operations.
Our primary assets are the units of partnership interest in Omega OP and, as a result, we will depend on distributions from Omega OP to pay dividends and expenses.
The Company is a holding company and has no material assets other than units of partnership interest in Omega OP. We intend to cause the partnership to make distributions to its partners, including the Company, in an amount sufficient to allow us to qualify as a REIT for U.S. federal income tax purposes and to pay all of our expenses. To the extent we need funds and the partnership is restricted from making distributions under applicable law or otherwise, or if the partnership is otherwise unable to provide such funds, the failure to make such distributions could materially adversely affect our liquidity and financial condition.
Members of our management and Board are holders of units of partnership interest in Omega OP, and their interests may differ from those of our public stockholders.
Some members of our management and Board hold partnership interest in Omega OP. Those unitholders may have conflicting interests with holders of the Company’s common stock. For example, such unitholders of Omega OP Units may have different tax positions from the Company or holders of our common stock, which could influence their decisions in their capacities as members of management regarding whether and when to dispose of assets, whether and when to incur new or refinance existing indebtedness and how to structure future transactions.
Our investments in joint ventures could be adversely affected by shared decision-making authority, our joint venture partners’ financial condition, and our exposure to potential losses from the actions of our joint venture partners.
As of December 31, 2021, we have ownership interest in one consolidated joint venture and several unconsolidated joint ventures. These joint ventures involve additional risks, including the following:
| ● | We may be unable to take actions that are opposed by our joint venture partners under arrangements that require us to share decision-making authority over major decisions affecting the ownership or operation of the joint venture and any property owned by the joint venture, such as the sale or financing of the property, our ability to sell or transfer our interest in a joint venture or the making of additional capital contributions for the benefit of the property; |
| ● | For joint ventures in which we have a noncontrolling interest, our joint venture partners may take actions that we oppose; |
| ● | Our joint venture partners may become bankrupt or fail to fund their share of required capital contributions, which could delay construction or development of a property or increase our financial commitment to the joint venture; |
| ● | Our joint venture partners may have business interests or goals with respect to a property that conflict with our business interests and goals, including with respect to the timing, terms and strategies for investment, which could increase the likelihood of disputes regarding the ownership, management or disposition of the property; |
| ● | Disagreements with our joint venture partners could result in litigation or arbitration that increases our expenses, distracts our officers and directors, and disrupts the day-to-day operations of the property, including by delaying important decisions until the dispute is resolved; and |
| ● | We may suffer losses resulting from actions taken by our joint venture partners with respect to our joint venture investments. |
28
Risks Related to Taxation
Qualifying as a REIT involves highly technical and complex provisions of the Code; failure to qualify as a REIT would subject us to increased taxes and impair our ability to expand our business and make distributions; and complying with REIT requirements may affect our profitability.
We were organized to qualify for taxation as a REIT under Sections 856 through 860 of the Code. See Item 1. Business – Taxation of Omega. Qualification as a REIT involves the application of technical and intricate Code provisions for which there are only limited judicial and administrative interpretations, and which involve the determination of various factual matters and circumstances not entirely within our control. We cannot assure that we will at all times satisfy these rules and tests. Even a technical or inadvertent violation could jeopardize our REIT qualification.
If we were to fail to qualify as a REIT in any taxable year, as a result of a determination that we failed to meet the annual distribution requirement or otherwise, we would be subject to federal corporate income tax, and any applicable alternative minimum tax with respect to each such taxable year for which the statute of limitations remains open, as well certain excise taxes on nonqualified REIT income, or disqualification from treatment as a REIT for the four taxable years following the year during which qualification is lost. This treatment would significantly reduce our net earnings and cash flow because of our additional tax liability for the years involved, which could significantly impact our financial condition. We generally must distribute annually at least 90% of our taxable income to our stockholders to maintain our REIT status. To the extent that we do not distribute all of our net capital gain or do distribute at least 90%, but less than 100% of our “REIT taxable income,” as adjusted, we will be subject to tax thereon at regular ordinary and capital gain corporate tax rates. As a result of all these factors, our failure to maintain our qualification as a REIT could impair our ability to expand our business and raise capital, and would substantially reduce our ability to make distributions to you.
To qualify as a REIT for federal income tax purposes, we must continually satisfy tests concerning, among other things, the nature and diversification of our assets, the sources of our income and the amounts we distribute to our stockholders. Thus, we may be required to liquidate otherwise attractive investments from our portfolio or be unable to pursue investments that would be otherwise advantageous to us, to satisfy the asset and income tests or to qualify under certain statutory relief provisions. We may also be required to make distributions to stockholders at disadvantageous times or when we do not have funds readily available for distribution (e.g., if we have assets which generate mismatches between taxable income and available cash). Having to comply with the distribution requirement could cause us to: (i) sell assets in adverse market conditions; (ii) borrow on unfavorable terms; or (iii) distribute amounts that would otherwise be invested in future acquisitions, capital expenditures or repayment of debt. As a result, satisfying the REIT requirements could have an adverse effect on our business results and profitability.
There is a risk of changes in the tax law applicable to REITs.
The Internal Revenue Service, the U.S. Treasury Department and Congress frequently review U.S. federal income tax legislation, regulations and other guidance. We cannot predict whether, when or to what extent new U.S. federal tax laws, regulations, interpretations or rulings will be adopted. Any legislative action may prospectively or retroactively modify our tax treatment and, therefore, may adversely affect taxation of us, our properties, or our shareholders.
Risks Related to Our Stock and Capital Structure
Our issuance of additional capital stock, warrants or debt securities, whether or not convertible, may reduce the market price for our outstanding securities, including our common stock, and dilute the ownership interests of existing stockholders, and we may issue securities with greater dividend, liquidation and other rights than our common stock.
We cannot predict the effect, if any, that future sales of our capital stock, warrants or debt securities, or the availability of our securities for future sale, will have on the market price of our securities, including our common stock. Sales of substantial amounts of our common stock or preferred shares, warrants or debt securities convertible into or exercisable or exchangeable for common stock in the public market, or the perception that such sales might occur, could negatively impact the market price of our stock and the terms upon which we may obtain additional equity financing in the future. Our Board has the authority to designate and issue preferred stock that may have dividend, liquidation and other rights that are senior to those of our common stock.
29
Any debt securities, preferred shares, warrants or other rights to acquire shares or convertible or exchangeable securities that we issue in the future may have some rights, preferences and privileges more favorable than those of our common stock and may result in dilution to owners of our common stock. Holders of our common stock are not entitled to preemptive rights or other protections against dilution. Our preferred shares, if issued, could have a preference on liquidating distributions or a preference on dividend payments that could limit our ability pay dividends or other distributions to the holders of our common stock. Because our decision to issue securities in any future offering will depend on market conditions and other factors beyond our control, we cannot predict or estimate the amount, timing or nature of our future offerings. Thus, our stockholders bear the risk that our future offerings could reduce the per share trading price of our common stock and dilute their interest in us.
General Risk Factors
Our success depends in part on our ability to retain key personnel and our ability to attract or retain other qualified personnel.
Our future performance depends to a significant degree upon the continued contributions of our executive management team and other key employees, the loss of whom could have an adverse impact on our operations. Although we have entered into employment agreements with the members of our executive management team, these agreements may not assure their continued service. In addition, our failure to successfully attract, hire, retain and train the people we need may impede our ability to implement our business strategy.
We rely on information technology in our operations, and any material failure, inadequacy, interruption or security failure of that technology could harm our business.
We rely on information technology networks and systems, including the Internet, to process, transmit and store electronic information, and to manage or support a variety of business processes, including financial transactions and records, personal identifying information, tenant and lease data. In addition, we may from time to time offer technology services to tenants, which may involve storage of customer or resident data. We purchase some of our information technology from vendors, on whom our systems depend. We generally rely on third-party systems, software, tools and monitoring to provide security for processing, transmission and storage of confidential tenant and other customer information, such as individually identifiable information, including information relating to financial accounts. It is possible that our safety and security measures will not be able to prevent the systems’ improper functioning or the improper access or disclosure of personally identifiable information such as in the event of cyber-attacks. Security breaches, including physical or electronic break-ins, computer viruses, attacks by hackers and similar breaches, can create system disruptions, shutdowns or unauthorized disclosure of confidential information. Any failure to maintain proper function, security and availability of our information systems, and the privacy of the data we store, or failure to comply with related regulations, could interrupt our operations, damage our reputation, subject us to liability claims or regulatory penalties and could have a material adverse effect on our business, financial condition and results of operations. The regulatory environment related to cyber and information security, data collection and privacy is increasingly rigorous, with new and constantly changing requirements applicable to our business or to which we may become subject, including E.U. data protection legislation, such as they General Data Protection Regulation, or the GDPR, and the U.K.’s Data Protection Act, which impose significant data protection requirements and penalties for noncompliance. Compliance with any of these requirements may result in additional costs and could impact how we conduct in business in new jurisdictions.
Failure to maintain effective internal control over financial reporting could have a material adverse effect on our business, results of operations, financial condition and stock price.
We are required to provide a report by management on internal control over financial reporting, including management’s assessment of the effectiveness of such control. Changes to our business will necessitate ongoing changes to our internal control systems and processes, and internal control over financial reporting may not prevent or detect misstatements due to inherent limitations, including the possibility of human error, the circumvention or overriding of controls, or fraud. Therefore, even effective internal controls can provide only reasonable assurance with respect to the preparation and fair presentation of financial statements. If we fail to maintain the adequacy of our internal controls or to implement required new or improved controls, our business, results of operations and financial condition could be materially adversely harmed, we could fail to meet our reporting obligations and there could be a material adverse effect on our stock price. In addition, we may be adversely impacted by new accounting pronouncements which change our lease recognition or other accounting practices or otherwise alter how we report our financial results, or which require that we change our internal control and operating procedures, which we may be unable to do in a timely manner.
Item 1B – Unresolved Staff Comments
None.
30
Item 2 – Properties
At December 31, 2021, our real estate investments include SNFs and ALFs and to a lesser extent ILFs, specialty facilities and MOBs, in the form of (i) owned facilities that are leased to operators or their affiliates, (ii) investments in direct financing leases to operators or their affiliates and (iii) mortgages on facilities that are operated by the mortgagors or their affiliates. The properties are located in 42 states and the U.K.
The following table presents the concentration of our real estate investments by state and the U.K. as of December 31, 2021:
% of |
|
|||||||||
Gross Real Estate |
Gross Real |
|
||||||||
Number of |
Number of |
Investment |
Estate |
|
||||||
Location |
|
Operating Beds |
|
Facilities |
|
(in thousands) |
|
Investment |
|
|
Florida |
|
16,345 |
|
133 |
$ |
1,491,905 |
|
14.7 |
% |
|
Texas |
|
11,190 |
|
114 |
|
995,386 |
|
9.8 |
% |
|
Michigan |
|
4,833 |
|
46 |
|
648,738 |
|
6.4 |
% |
|
Indiana |
|
6,941 |
|
70 |
|
643,640 |
|
6.4 |
% |
|
California |
|
4,476 |
|
53 |
|
580,542 |
|
5.7 |
% |
|
Ohio |
|
4,957 |
|
48 |
|
579,343 |
|
5.7 |
% |
|
Pennsylvania |
|
4,960 |
|
54 |
|
554,741 |
|
5.5 |
% |
|
United Kingdom |
|
3,057 |
|
59 |
|
447,574 |
|
4.4 |
% |
|
Virginia |
|
3,668 |
|
28 |
|
422,024 |
|
4.2 |
% |
|
New York |
|
258 |
|
1 |
|
336,069 |
|
3.3 |
% |
|
Remaining States |
|
35,018 |
|
354 |
|
3,430,983 |
|
33.9 |
% |
|
95,703 |
960 |
$ |
10,130,945 |
100.0 |
% |
|||||
Item 3 – Legal Proceedings
See Note 20— Commitments and Contingencies to the Consolidated Financial Statements - Part IV, Item 15, which is hereby incorporated by reference in response to this item.
Item 4 – Mine Safety Disclosures
None.
PART II
Item 5 – Market for the Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
Market Information
Shares of Omega Healthcare Investors, Inc. (together with its consolidated subsidiaries, collectively, “Omega” or the “Company”) common stock are traded on the New York Stock Exchange under the symbol “OHI.” As of February 11, 2022, there were 2,755 registered holders and 239,112,249 shares of Omega common stock outstanding.
Performance Graph
The graph and table below compare the cumulative total return of Omega, the FTSE NAREIT Equity Health Care Index (Ticker: FN11-FTX), the FTSE NAREIT All REITs Index (Ticker: FNAR), the S&P 500 Index, and the Russell 2000 from January 1, 2017 to December 31, 2021. We have included the FTSE NAREIT Equity Health Care Index and the FTSE NAREIT All REITs Index because we believe that they are representative of the industry in which we compete and are relevant to an assessment of our performance. Total cumulative return is based on a $100 investment in Omega common stock and in each of the indices at the close of trading on December 31, 2016 and assumes quarterly reinvestment of dividends. Stockholder returns over the indicated periods should not be considered indicative of future stock prices or stockholder returns.
31
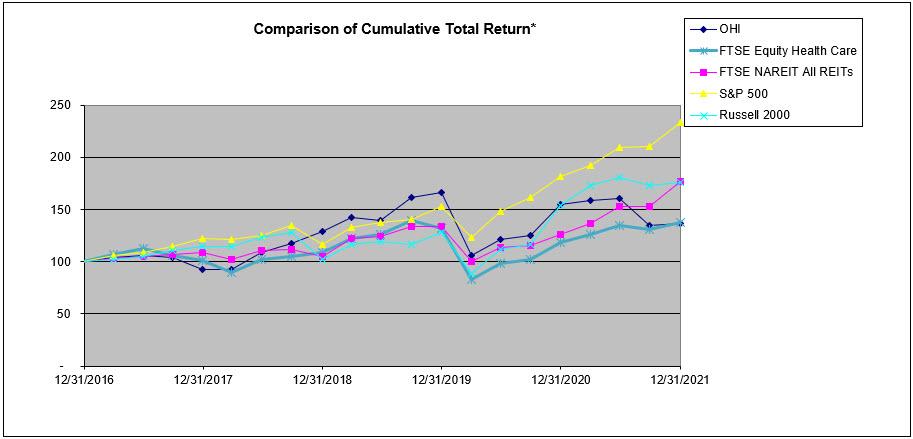
12/31/2016 |
12/31/2017 |
12/31/2018 |
12/31/2019 |
12/31/2020 |
12/31/2021 |
|||||||||||||
Omega Healthcare Investors, Inc. |
$ |
100.00 |
$ |
92.23 |
$ |
128.60 |
$ |
166.07 |
$ |
154.47 |
$ |
136.26 |
||||||
FTSE NAREIT Health Care Index |
$ |
100.00 |
$ |
100.88 |
$ |
108.52 |
$ |
131.51 |
$ |
118.54 |
$ |
137.90 |
||||||
FTSE NAREIT All REITs Index |
$ |
100.00 |
$ |
109.27 |
$ |
104.79 |
$ |
134.20 |
$ |
126.33 |
$ |
176.71 |
||||||
S&P 500 Index |
$ |
100.00 |
$ |
121.83 |
$ |
116.49 |
$ |
153.17 |
$ |
181.35 |
$ |
233.41 |
||||||
Russell 2000 Index |
$ |
100.00 |
$ |
114.65 |
$ |
102.02 |
$ |
128.06 |
$ |
153.62 |
$ |
176.39 |
||||||
Issuer Purchases of Equity Securities
On March 20, 2020, the Company authorized the repurchase of up to $200 million of our outstanding common stock from time to time over the twelve months ending March 20, 2021. Omega did not repurchase any of its stock under this amended program during 2020 and 2021.
On January 27, 2022, the Company authorized the repurchase of up to $500 million of our outstanding common stock from time to time through March 2025. The Company is authorized to repurchase shares of its common stock in open market and privately negotiated transactions or in any other manner as determined by the Company’s management and in accordance with applicable law. The timing and amount of stock repurchases will be determined, in management’s discretion, based on a variety of factors, including but not limited to market conditions, other capital management needs and opportunities, and corporate and regulatory considerations. The Company has no obligation to repurchase any amount of its common stock, and such repurchases, if any, may be discontinued at any time.
During 2021, we did not repurchase any shares of our outstanding common stock.
32
Unregistered Sales of Equity Securities and Use of Proceeds
During the quarter ended December 31, 2021, Omega issued an aggregate of 12,985 shares of Omega common stock in exchange for an equivalent number of units of partnership interest in OHI Healthcare Properties Limited Partnership (collectively with subsidiaries, “Omega OP”) tendered to Omega OP for redemption in accordance with the provisions of its partnership agreement. The Company issued these shares of Omega common stock in reliance on an exemption from registration under Section 4(a)(2) of the Securities Act of 1933, as amended, based upon factual representations received from the limited partners who received the Omega common stock.
Item 6 – [Reserved]
Item 7 – Management’s Discussion and Analysis of Financial Condition and Results of Operations
The following discussion and analysis is based primarily on the consolidated financial statements of Omega Healthcare Investors, Inc. presented in conformity with U.S. generally accepted accounting principles (“GAAP”) for the periods presented and should be read together with the notes thereto contained in this Annual Report on Form 10-K. Other important factors are identified in “Forward-Looking Statements” and “Item 1A - Risk Factors” above.
Overview and Outlook
Omega Healthcare Investors, Inc. (“Parent”) is a Maryland corporation that, together with its consolidated subsidiaries has elected to be taxed as a REIT for federal income tax purposes. Omega is structured as an umbrella partnership REIT (“UPREIT”) under which all of Omega's assets are owned directly or indirectly by, and all of Omega's operations are conducted directly or indirectly through, its operating partnership subsidiary, Omega OP. As of December 31, 2021, Parent owned approximately 97% of the issued and outstanding units of partnership interest in Omega OP (“Omega OP Units”), and other investors owned approximately 3% of the outstanding Omega OP Units.
Omega has one reportable segment consisting of investments in healthcare-related real estate properties located in the United States (“U.S.”) and the United Kingdom (“U.K.”). Our core business is to provide financing and capital to the long-term healthcare industry with a particular focus on skilled nursing facilities (“SNFs”), assisted living facilities (“ALFs”), and to a lesser extent, independent living facilities (“ILFs”), rehabilitation and acute care facilities (“specialty facilities”) and medical office buildings (“MOBs”). Our core portfolio consists of our long-term leases and mortgage loans with healthcare operating companies and affiliates (collectively, our “operators”). All of our leases to our operators are “triple-net” leases, which require the operators to pay all property-related expenses. All of our mortgages are secured by first liens on the underlying real estate and personal property of the operators. In addition to our core investments, we selectively make loans to operators for working capital and capital expenditures. These loans, which may be either unsecured or secured by the collateral of the borrower, are classified as other investments. From time to time, we also acquire equity interests in joint ventures or entities that support the long-term healthcare industry and our operators.
Our portfolio of investments at December 31, 2021, included 960 healthcare facilities, located in 42 states and the U.K. that are operated by 63 third-party operators. Our real estate investment in these facilities totaled approximately $10.1 billion at December 31, 2021, with approximately 98% of our real estate investments related to long-term healthcare facilities. The portfolio is made up of (i) 685 SNFs, (ii) 133 ALFs, (iii) 20 ILFs, (iv) 16 specialty facilities, (v) two MOBs, (vi) fixed rate mortgages on 59 SNFs, two ALFs and two specialty facilities and (vii) 41 facilities that are held for sale. At December 31, 2021, we held other investments of approximately $469.9 million, consisting primarily of secured loans to third-party operators of our facilities and $194.7 million of investments in six unconsolidated joint ventures.
As healthcare delivery continues to evolve, we continuously evaluate potential investments, our assets, operators and markets to position our portfolio for long-term success. Our strategy includes applying data analytics to our investment underwriting and asset management, as well as selling or transitioning assets that do not meet our portfolio criteria.
33
COVID-19 Pandemic Update
The COVID-19 pandemic has significantly and adversely impacted SNFs and long-term care providers due to the higher rates of virus transmission and fatality among the elderly and frail populations that these facilities serve. As a result, many of our operators have been and may continue to be significantly impacted by the pandemic. During the third and fourth quarters of 2020, four of our operators, including Agemo Holdings, LLC (“Agemo”) and Genesis Healthcare, Inc. (“Genesis”), indicated in their financial statements substantial doubt regarding their ability to continue as going concerns, citing in part the impact of the COVID-19 pandemic and uncertainties regarding the continuing availability of sufficient government support. This resulted in placing these operators on a cash basis of revenue recognition and a corresponding write-off of approximately $143.0 million in aggregate of contractual receivables, straight-line receivables and lease inducements to rental income during fiscal year 2020. During the year ended December 31, 2021, Agemo, Gulf Coast Health Care LLC (together with certain affiliates “Gulf Coast”), Guardian Healthcare (”Guardian”) and one other operator either failed to make contractual rent or interest payments for a period or have informed us that they would be unable to pay us rent for the foreseeable future. See “Portfolio and Recent Developments – Guardian” below. In addition, on October 14, 2021, Gulf Coast commenced voluntary cases under chapter 11 of the U.S. Bankruptcy Code. See “Receivables, Other Investments and Operator Collectibility – Gulf Coast” below. As of December 31, 2021, we have placed six operators, inclusive of Gulf Coast, Guardian and the one other non-paying operator noted above, on a cash basis of revenue recognition during 2021 as collection of substantially all contractual lease payments with these six operators was no longer probable.
We believe these operators were impacted by, among other things, reduced revenue as a result of lower occupancy and increased expenses resulting from the COVID-19 pandemic and uncertainties regarding the continuing availability of sufficient government support. In connection with these developments, we wrote off approximately $36.0 million in aggregate of straight-line receivables and lease inducements to rental income for the year ended December 31, 2021 (in connection with the six operators placed on a cash basis during the year). We have also have taken impairments of $83.4 million for the year ended December 31, 2021 in connection with loans outstanding with Agemo, Gulf Coast and Guardian, all of whom are non-paying operators. The six operators that were placed on a cash basis during 2021 collectively represent 6.6% and 7.3%, respectively, of our total revenues (excluding the impact of the write-offs in 2021 and 2020) for the years ended December 31, 2021 and 2020. We remain cautious as the COVID-19 pandemic continues to have a significant impact on our operators and their financial conditions, particularly given continued uncertainty regarding the availability of sufficient government support, the persistence of staffing shortages that continue to impact our operators’ occupancy levels and profitability, the impact of governmental vaccine mandates for staff on these ongoing staffing shortages, other factors that may impact virus transmission in our facilities, including genetic mutations of the virus into new variants, the commencement in April 2021 for many of our operators of the repayment of accelerated payments of Medicare funds that were previously received as Advanced Medicare payments in 2020 and the commencement in December 2021 of repayment of deferred FICA obligations.
As of January 26, 2022, our operators reported cases of COVID-19 within 713, or 75.5%, of our 944 operating facilities as of September 30, 2021, which includes cases involving employees and residents. This represents a significant increase from the 263 facilities with cases, or 27.7%, of our 949 operating facilities, that our operators reported as of October 27, 2021. Consistent with national trends, we experienced a slight downturn in the number of COVID-19 cases in our facilities from September to November of 2021, followed by a slight increase in December and a meaningful increase in January driven by new variants. The January 2022 case counts are consistent with case rates that were experienced in January 2021, which represented an increase over the December 22, 2020 cases in 614 facilities, or 64% of our 959 operating facilities. We caution that we have not independently validated any such facility virus incidence information, which may be reported on an inconsistent basis by our operators, and we can provide no assurance regarding the information’s accuracy or that there have not been any changes since the time it was obtained from our operators; we also undertake no duty to update this information. It remains uncertain when and to what extent vaccination programs for COVID-19 and any booster doses will mitigate the effects of COVID-19 in our facilities, particularly with regard to new variants of the virus, the impact of governmental vaccine mandates for staff on ongoing staffing shortages in our facilities and other factors that impact virus transmission in our facilities. The impact of these programs will depend in part on the continued efficacy and delivery of the vaccine and booster doses in our facilities, compliance with staff vaccination requirements and participation levels in vaccination programs among the residents and employees of our operators and in the communities in which they operate.
34
In addition to experiencing outbreaks of positive cases and deaths of residents and employees during the pandemic, our operators have been required to, and continue to, adapt their operations to manage the spread of the COVID-19 virus as well as the implementation of new treatments and vaccines, and to implement new requirements relating to infection control, staffing levels, personal protective equipment (“PPE”), testing mandates, quality of care, visitation protocols and reporting, among other regulations, throughout the pandemic while facing staffing shortages that have accelerated during the pandemic and that may impede the delivery of care. Many of our operators have reported incurring significant cost increases as a result of the COVID-19 pandemic, with dramatic increases for facilities with positive cases. These increases have been offset to some extent by increases in reimbursements due to increased skilling in place, which has been necessitated by pandemic-related protocols and may decrease when such protocols subside. We believe these increases primarily stem from elevated labor costs, including increased use of overtime and bonus pay and reliance on agency staffing due to staffing shortages, as well as a significant increase in both the cost and usage of PPE, testing equipment and processes and supplies, as well as implementation of new infection control protocols and vaccination programs. The federal government announced in August and September 2021 that it would be requiring SNF and healthcare workers to be vaccinated against COVID-19 and issued an emergency implementing regulation effective November 5, 2021 requiring covered healthcare facilities to ensure eligible staff have received a first vaccine dose as of December 5, 2021 and a second dose of a two-dose vaccine as of January 4, 2022, with certain permitted exemptions in alignment with federal law, which were subsequently extended by the U.S. Centers for Medicare and Medicaid Services by between one to two months depending on the applicable state. Notwithstanding these extensions, vaccination rates have increased in anticipation of the full implementation of the requirements and we expect them to further increase once such requirements are fully implemented. However, we expect that such mandates may exacerbate ongoing staffing shortages in skilled nursing and senior housing facilities. In addition, operators who do not achieve full compliance with the requirements may face potential survey issues and penalties. At this time, there is significant uncertainty regarding the impact of such developments. In addition, our facilities, on average, have experienced declines, in some cases that are material, in occupancy levels as a result of the pandemic. While these declines have generally improved on average during 2021, new variants have caused improvement in occupancy to stall towards the end of 2021 and average occupancy has not returned to pre-pandemic levels. It remains unclear when and the extent to which demand and occupancy levels will return to pre-COVID-19 levels. We believe these challenges to occupancy recovery may be in part due to staffing shortages, which in some cases have required operators to limit admissions, as well as COVID-19 related fatalities at the facilities, the delay of SNF placement and/or utilization of alternative care settings for those with lower level of care needs, the suspension and/or postponement of elective hospital procedures, fewer discharges from hospitals to SNFs and higher hospital readmittances from SNFs.
While substantial government support, primarily through the federal CARES Act in the U.S. and distribution of PPE, vaccines and testing equipment by federal and state governments, was allocated to SNFs and to a lesser extent to ALFs in 2020, federal relief efforts were limited in 2021 as have been relief efforts in certain states. We believe further government support will be needed to continue to offset these impacts. It is unclear whether and to what extent such government support will continue to be sufficient and timely to offset these impacts. In particular, while $25.5 billion in federal funding for healthcare providers impacted by COVID-19 was announced in September 2021 with distributions beginning in late 2021, it remains unclear the extent to which these funds or remaining unallocated funds under the Public Health and Social Services Emergency Fund (“Provider Relief Fund”) will be distributed to our operators in any meaningful way, whether additional funds will be added to the Provider Relief Fund or otherwise allocated to healthcare operators or our operators, or whether additional Medicaid funds under the American Rescue Plan Act of 2021 (the “American Rescue Plan Act”) in the U.S. will ultimately support reimbursement to our operators. Further, to the extent the cost and occupancy impacts on our operators continue or accelerate and are not offset by continued government relief that is sufficient and timely, we anticipate that the operating results of additional operators may be materially and adversely affected, some may be unwilling or unable to pay their contractual obligations to us in full or on a timely basis and we may be unable to restructure such obligations on terms as favorable to us as those currently in place.
There are a number of uncertainties we face as we consider the potential impact of COVID-19 on our business, including how long census disruption and elevated COVID-19 costs will last, the impact of vaccination programs, including booster doses, and participation levels in those programs in reducing the spread of COVID-19 in our facilities, the impact of genetic mutations of the virus into new variants on our facilities, the impact of vaccine mandates on ongoing staffing shortages in our facilities, and the extent to which funding support from the federal government and the states will continue to offset these incremental costs as well as lost revenues. Notwithstanding vaccination programs, we expect that heightened clinical protocols for infection control within facilities will continue for some period; however, we do not know if future reimbursement rates or equipment provided by governmental agencies will be sufficient to cover the increased costs of enhanced infection control and monitoring.
35
While we continue to believe that longer term demographics will drive increasing demand for needs-based skilled nursing care, we expect the uncertainties to our business described above to persist at least for the near term until we can gain more information as to the level of costs our operators will continue to experience and for how long, and the level of additional governmental support that will be available to them, the potential support our operators may request from us and the future demand for needs-based skilled nursing care and senior living facilities. We continue to monitor the rate of occupancy recovery at many of our operators, and it remains uncertain whether and when demand, staffing availability and occupancy levels will return to pre-COVID-19 levels.
We continue to monitor the impacts of other regulatory changes, as discussed in Item 1. Business – Government Regulation and Reimbursement, including any significant limits on the scope of services reimbursed and on reimbursement rates and fees, which could have a material adverse effect on an operator’s results of operations and financial condition, which could adversely affect the operator’s ability to meet its obligations to us.
Other Trends and Conditions
In addition to the impacts of COVID-19 discussed above, our operations have also been and may continue to be impacted by increased competition for the acquisition of facilities in the U.S., which has decreased the number of investment opportunities that would be accretive to our portfolio. As part of our continuous evaluation of our portfolio and in connection with certain operator workout transactions, we expect to continue to opportunistically sell assets, or portfolios of assets, from time to time.
2021 and Recent Highlights
Investments
| ● | We acquired 32 facilities for an aggregate consideration of $604.0 million during the year ended December 31, 2021. The initial cash yield (the initial annual contractual cash rent divided by the purchase price) on these asset acquisitions was between 7.89% and 9.25%. This includes the acquisition of 24 facilities from Healthpeak Properties, Inc. (“Healthpeak”) for $511.3 million in the first quarter. We also had $58.6 million of non-cash acquisitions of facilities previously subject to mortgage loans with Omega in which principal amounts under the loan agreements were reduced or settled in exchange for title to the facilities. |
| ● | We invested $140.0 million under our construction-in-progress and capital improvement programs during the year ended December 31, 2021. This includes the purchase of a real estate property located in Washington, D.C. in the third quarter for approximately $68.0 million that Omega, in conjunction with Maplewood Senior Living (along with affiliates, “Maplewood”), plans to redevelop into a 174-bed ALF and lease back to Maplewood. |
| ● | We financed $82.5 million of new mortgage loans for eight facilities with a weighted average interest rate of 10.3%. In 2021, we also advanced $4.2 million under existing mortgage loans. |
Dispositions and Impairments
| ● | In 2021, we sold 48 facilities for approximately $318.5 million in net cash proceeds, recognizing a net gain of approximately $161.6 million. |
| ● | In 2021, we recorded impairments on real estate properties of approximately $44.7 million on 14 facilities primarily as a result of reclassifying facilities to held for sale. |
| ● | In 2021, we terminated the Daybreak Ventures, LLC (“Daybreak”) master lease and fully exited our relationship after transitioning 14 Daybreak facilities to existing operators and selling the four remaining Daybreak facilities. |
| ● | In December 2021, we entered into an agreement to sell 22 facilities that were previously leased and operated by Gulf Coast Health Care LLC (together with certain affiliates “Gulf Coast”) for estimated gross proceeds of $317.5 million. The agreement includes an earnout clause pursuant to which the buyer is obligated to pay an additional $18.7 million to Omega if certain financial metrics are achieved at the facilities in the five years following the sale. The sale is targeted to close on or around April 1, 2022. See “Collectibility Issues” below for further developments related to Gulf Coast. |
36
Financing Activities
| ● | On March 10, 2021, the Company issued $700 million aggregate principal amount of its 3.250% Senior Notes due 2033. The notes were sold at a public offering price of 99.304% of their face value before the underwriters’ discount. The Company’s net proceeds from the offering were used to repay $350 million of aggregate principal of our 4.375% Senior Notes due 2023 on March 18, 2021 and partially repay borrowings under the Company’s then outstanding revolving credit facility and term loans. As a result of the notes retirement, the Company recorded approximately $30.8 million in early extinguishment of debt charges. |
| ● | On April 30, 2021, the Company entered into a new four-year $1.45 billion senior unsecured credit facility (the “Revolving Credit Facility”). The Revolving Credit Facility replaced a $1.25 billion senior unsecured credit facility that was scheduled to mature on May 25, 2021. |
| ● | On April 30, 2021, the Company’s operating partnership subsidiary entered into a new four-year $50 million senior unsecured term loan facility (the “OP Term Loan”). The OP Term Loan replaced a $50 million senior unsecured term loan that was scheduled to mature on May 25, 2022. |
| ● | On May 13, 2021, we established a $1.0 billion at-the-market program (the “2021 ATM Program”) to sell shares of our common stock from time to time in an at-the-market offering. The 2021 ATM Program replaced our $500 million Equity Shelf Program that was entered into in 2015 (the “2015 ATM Program”). |
| ● | We sold 7.6 million shares of common stock under our 2015 ATM Program, 2021 ATM Program and Dividend Reinvestment and Common Stock Purchase Plan (“DRSPP”) during the year ended December 31, 2021. Aggregate net proceeds from these sales generated $278.4 million during 2021. |
Other Highlights
| ● | In January 2022, our Board authorized the repurchase of up to $500 million of our outstanding common stock, from time to time, through March 2025. |
| ● | During 2021, we made $62.1 million of new other investment loans with a weighted average interest rate of 9.3%. In 2021, we also advanced $88.4 million under existing other investment loans. |
| ● | In the third quarter of 2021, we made an investment of $20.0 million in SafelyYou, Inc. (“SafelyYou”), a technology company that has developed artificial intelligence-enabled video that detects and helps prevent resident falls in ALFs and SNFs. Through our investment, we obtained preferred shares representing 5% of the outstanding equity of SafelyYou and warrants to purchase SafelyYou common stock representing an additional 5% of outstanding equity as of the date of our investment, which are subject to vesting conditions based on SafelyYou’s deployment of our invested capital to support Omega facilities and operators. As part of our investment strategy, we will continue to evaluate investments in companies that provide complementary products and services that improve the quality of our facilities and allow our operators to improve care. |
| ● | In 2021, Omega was included in the Bloomberg Gender-Equality Index (GEI) – one of only 380 companies worldwide, and fewer than 15 U.S. REITs, to be included in the 2021 index. |
37
Collectibility Issues
| ● | During the second quarter of 2021, Gulf Coast stopped paying contractual rent under its master lease agreement for 24 facilities because of on-going liquidity issues. On October 14, 2021, Gulf Coast commenced voluntary cases under chapter 11 of the U.S. Bankruptcy Code. As a result of Gulf Coast’s non-payment of contractual rent, in the second quarter of 2021, we placed Gulf Coast on a cash basis of revenue recognition and wrote-off straight-line rent receivable balances of $17.4 million through rental income. Subsequent to placing Gulf Coast on a cash basis of revenue recognition in June 2021, we recognized $24.6 million of contractual rent during the remaining period of 2021, based on our ability to offset any uncollected rent receivables against Gulf Coast’s security deposit and against certain debt obligations of Omega. In connection with the bankruptcy, we agreed to provide up to $25.0 million in senior secured debtor-in-possession (“DIP”) financing to Gulf Coast, subject to certain conditions, to provide liquidity and assist with the transition of operations in our 23 open facilities. Operations of the 23 open facilities were transitioned to a new manager on December 1, 2021 for an interim period until the license for the facilities could be obtained by a new operator. In the fourth quarter of 2021, we funded $20.5 million under the DIP facility and fully reserved for the loan principal through the provision for credit losses. During the Interim Period, no rent is being paid by Gulf Coast, and we have provided a $20.0 million working capital loan to the new manager, discussed in further detail in Note 8 – Other Investments to our Consolidated Financial Statements. |
| ● | From August 2021 through October 2021 and December 2021, Agemo Holdings, LLC (“Agemo”) failed to pay contractual rent and interest due under their lease and loan agreements, but paid rent and interest in November 2021. As of December 31, 2021, we have two loans outstanding to Agemo, a term loan with remaining principal of $32.0 million that bears interest at 9% per annum and matures on December 31, 2024 (the “Agemo Term Loan”) and a $25.0 million secured working capital loan bearing interest at 7% per annum that matures on April 30, 2025 (the “Agemo WC Loan”). In the third quarter of 2021, we recorded a provision for credit losses of $16.7 million related to these loans as a result of a reduction in the fair value of the underlying collateral assets supporting the current carrying values. During the third and fourth quarters of 2021, we recorded $8.7 million of revenue by collecting rental and interest payments and we recorded $8.5 million of revenue by drawing on the letter of credit and through application of the security deposit balance. |
| ● | From October 2021 through December 2021, Guardian Healthcare (“Guardian”) failed to make contractual rent and interest payments under its lease agreement for 26 operating facilities and on its $112.5 million mortgage loan agreement, bearing interest at 10.81%, for nine facilities, due to ongoing liquidity issues. As a result of Guardian’s non-payment of contractual rent, in the fourth quarter of 2021, we placed Guardian on a cash basis of revenue recognition and wrote off approximately $14.0 million of straight-line rent receivables and lease inducements through rental income. As of December 31, 2021, we have $7.4 million of letters of credit from Guardian as collateral which could be applied against our uncollected rent and interest receivables. On December 30, 2021, we acquired two facilities, previously subject to the Guardian mortgage loan, in consideration for a reduction of $8.7 million in the mortgage principal and added the facilities to the master lease agreement. During the fourth quarter of 2021, we concluded that the $112.5 million first mortgage loan was impaired. We recorded a provision for credit loss of $38.2 million during the fourth quarter of 2021 to reduce the carrying value of this loan to the fair value of the underlying collateral. See Note 9 – Allowance for Credit Losses to our Consolidated Financial Statements. |
| ● | In addition to the Gulf Coast and Guardian straight-line receivable write-offs in 2021 discussed above, during the year ended December 31, 2021, we wrote off straight-line rent receivable balances of $5.9 million through rental income primarily due to placing four other operators (one operator in the first quarter, two operators in the third quarter and one operator in the fourth quarter) on a cash basis of revenue recognition. We determined that collection of substantially all contractual lease payments with these operators was no longer probable. |
| ● | In January and February 2022, an operator, representing 3.4% of total revenue (excluded the impact of write-offs) for the year ended December 31, 2021, did not pay its contractual amounts due under its lease agreement. The operator asked for a short-term rent deferral and negotiations with the operator are on-going. Omega holds a $1.0 million letter of credit from this operator. The operator remains current on its loan obligations, which are secured by a first lien on the accounts receivable of the operator, as discussed further in Note 8 – Other Investments to our Consolidated Financial Statements. |
38
Dividends
| ● | On January 27, 2022, the Board of Directors declared a cash dividend for the quarter ended December 31, 2021 of $0.67 per share. |
Results of Operations
The following is our discussion of the consolidated results of operations for the year ended December 31, 2021 as compared to the year ended December 31, 2020. For a discussion of our results of operation for the year ended December 31, 2020 as compared to the year ended December 31, 2019, see “Item 7 – Management’s Discussion and Analysis of Financial Condition and Results of Operations” of our Form 10-K for the year ended December 31, 2020 (“2020 Form 10-K”).
Revenues
Our revenues for the year ended December 31, 2021 totaled $1.1 billion, an increase of $170.4 million over the same period in 2020. Following is a description of certain of the changes in revenues for the year ended December 31, 2021 compared to 2020:
| ● | Rental income was $923.7 million, an increase of $170.3 million over the same period in 2020. The increase was primarily the result of (i) $109.3 million increase due to a net reduction in straight-line rent receivable and lease inducement write-offs in 2021 following significant write-offs associated with Agemo and Genesis in the third quarter of 2020 as a result of placing these operators on a cash basis for revenue recognition, (ii) a $101.4 million increase related to facility acquisitions made in 2021 (primarily the 24 facilities acquired from Healthpeak in the first quarter), the completion of the construction of certain facilities that were placed in service in 2021 (primarily related to developmental projects with Maplewood), and incremental revenue as a result of transitioning facilities previously associated with Daybreak to other operators, (iii) a $7.7 million increase related to Gulf Coast as a result of accelerating rent due to a default under its master lease agreement and (iv) a $5.5 million one-time rent payment from a cash basis operator for past due contractual amounts owed under its lease agreement partially offset by a (a) $49.5 million decrease in rental income resulting from not recording straight-line rent for operators placed on a cash basis for revenue recognition in 2020 and 2021 and resulting from facility sales and (b) $4.7 million decrease related to the acceleration of the amortization of in-place lease intangibles resulting from facility transitions and lease terminations. |
| ● | Mortgage interest income totaled $91.7 million, an increase of $2.2 million over the same period in 2020. The increase was primarily due to new and refinanced mortgages and additional funding to existing operators made throughout 2020 and 2021, offset by principal payments. As noted above, in 2021, we funded $86.7 million for new or existing mortgages loans. |
Expenses
Our expenses for the year ended December 31, 2021, totaled $777.0 million, an increase of approximately $42.0 million over the same period in 2020. Following is a description of certain of the changes in our expenses for the year ended December 31, 2021 compared to 2020:
| ● | Our depreciation and amortization expense was $342.0 million for the year ended December 31, 2021, compared to $329.9 million for the same period in 2020. The increase primarily relates to the timing of facility acquisitions and capital expenditures, partially offset by a reduction in depreciation expense related to facility sales and facilities reclassified to assets held for sale. |
| ● | Our general and administrative (“G&A”) expense was $64.6 million, compared to $59.9 million for the same period in 2020. The increase primarily related to (i) a $2.6 million increase in stock-based compensation expense (see Note 19 – Stock-Based Compensation to the Consolidated Financial Statements for a full summary of stock-compensation movements over the last three years) and (ii) a $1.6 million increase in professional service costs related to the Gulf Coast bankruptcy and related matters. |
39
| ● | Our interest expense was $234.6 million, compared to $223.4 million for the same period in 2020. The increase primarily related to (i) interest on the $700 million senior notes issued in the fourth quarter of 2020 and (ii) interest on the $700 million senior notes issued in the first quarter of 2021, partially offset by the retirement of our previous $425 million senior unsecured U.S. Dollar term loan facility and our previous $250 million senior unsecured term loan facility in the fourth quarter of 2020, the partial paydown of our previous $50 million senior unsecured term loan obtained in 2017 in the fourth quarter of 2020, the redemption of $350 million of the 4.375% Senior Notes due 2023 and the repayment of outstanding borrowings on the 2017 Revolving Credit Facility and the Sterling term loan in the first quarter of 2021 and lower average borrowings under the Revolving Credit Facility. |
Other Income (Expenses)
For the year ended December 31, 2021, total other income was $130.3 million, an increase of approximately $125.4 million over the same period in 2020. The increase was primarily due to a $142.5 million increase in gain on assets sold – net resulting from the sale of 48 facilities and 43 facilities during 2021 and 2020, respectively, as we continue to exit certain facilities, operator relationships and/or states to improve the strength of our overall portfolio, offset by a $30.8 million loss on debt extinguishment primarily resulting from fees, premiums, and expenses related to the redemption of $350 million of the 4.375% Senior Notes due 2023 during the first quarter of 2021.
Income Tax Expense
As a REIT, we generally are not subject to federal income taxes on the REIT taxable income that we distribute to stockholders, subject to certain exceptions. For tax year 2021, we made common dividend payments of $637.6 million to satisfy REIT requirements relating to qualifying income. We have elected to treat certain of our active subsidiaries as TRSs. Our domestic TRSs are subject to federal, state and local income taxes at the applicable corporate rates. Our foreign TRSs are subject to foreign income taxes. As of December 31, 2021, one of our TRSs that is subject to income taxes at the applicable corporate rates had a net operating loss (“NOL”) carry-forward of approximately $10.6 million. The loss carry-forward is fully reserved as of December 31, 2021 with a valuation allowance due to uncertainties regarding realization.
Under current law, NOL carry-forwards generated up through December 31, 2017 may be carried forward for no more than 20 years, and our NOL carry-forwards generated in our taxable years ended after December 31, 2017 may be carried forward indefinitely. The Coronavirus Aid, Relief, and Economic Security Act (the “CARES Act”) modified the NOL carryback rules to permit the use of NOLs arising after December 31, 2017 and before January 1, 2021 to be carried back to recover taxes paid in prior tax periods. We do not anticipate that such changes will materially impact the computation of Omega’s taxable income, or the taxable income of any Omega entity, including our TRSs. We also do not expect that Omega or any Omega entity, including our TRSs, will realize a material tax benefit as a result of the changes to the provisions of the Code made by the CARES Act.
40
For the year ended December 31, 2021, we recorded approximately $1.4 million of federal, state and local income tax provision and approximately $2.4 million of tax provision for foreign income taxes. These amounts do not include any gross receipts or franchise taxes payable to certain states and municipalities.
Income from Unconsolidated Joint Ventures
For the year ended December 31, 2021, income from unconsolidated joint ventures was $16.1 million, an increase of approximately $9.9 million over the same period in 2020. The increase was primarily due to one of the joint ventures realizing a $14.9 million gain on sale of real estate investments during 2021.
National Association of Real Estate Investment Trusts Funds From Operations
We use funds from operations (“Nareit FFO”), a non-GAAP financial measure, as one of several criteria to measure the operating performance of our business. We calculate and report Nareit FFO in accordance with the definition of Funds from Operations and interpretive guidelines issued by the National Association of Real Estate Investment Trusts (“Nareit”). Nareit FFO is defined as net income (computed in accordance with GAAP), adjusted for the effects of asset dispositions and certain non-cash items, primarily depreciation and amortization and impairment on real estate assets, and after adjustments for unconsolidated partnerships and joint ventures and changes in the fair value of warrants. Adjustments for unconsolidated partnerships and joint ventures are calculated to reflect funds from operations on the same basis. Revenue recognized based on the application of security deposits and letters of credit or based on the ability to offset against other financial instruments is included within Nareit FFO. We believe that Nareit FFO is an important supplemental measure of our operating performance. As real estate assets (except land) are depreciated under GAAP, such accounting presentation implies that the value of real estate assets diminishes predictably over time, while real estate values instead have historically risen or fallen with market conditions. Nareit FFO was designed by the real estate industry to address this issue. Nareit FFO herein is not necessarily comparable to Nareit FFO of other REITs that do not use the same definition or implementation guidelines or interpret the standards differently from us.
We further believe that by excluding the effect of depreciation, amortization, impairment on real estate assets and gains or losses from sales of real estate, all of which are based on historical costs and which may be of limited relevance in evaluating current performance, Nareit FFO can facilitate comparisons of operating performance between periods and between other REITs. We offer this measure to assist the users of our financial statements in evaluating our financial performance under GAAP, and Nareit FFO should not be considered a measure of liquidity, an alternative to net income or an indicator of any other performance measure determined in accordance with GAAP. Investors and potential investors in our securities should not rely on this measure as a substitute for any GAAP measure, including net income.
The following table presents our Nareit FFO results for the years ended December 31, 2021 and 2020:
Year Ended December 31, |
|||||||
|
|
2021 |
|
2020 |
|||
(in thousands) |
|||||||
Net income (1)(2) |
$ |
428,302 |
$ |
163,545 |
|||
Deduct gain from real estate dispositions |
(161,609) |
(19,113) |
|||||
Deduct gain from real estate dispositions - unconsolidated joint ventures |
|
(14,880) |
|
(5,894) |
|||
|
251,813 |
|
138,538 |
||||
Elimination of non-cash items included in net income: |
|
|
|
|
|||
Depreciation and amortization |
|
342,014 |
|
329,924 |
|||
Depreciation – unconsolidated joint ventures |
|
12,285 |
|
14,000 |
|||
Add back impairments on real estate properties |
44,658 |
72,494 |
|||||
Add back impairments on real estate properties - unconsolidated joint ventures |
4,430 |
— |
|||||
Add back unrealized loss on warrants |
|
43 |
|
988 |
|||
Nareit FFO |
$ |
655,243 |
$ |
555,944 |
|||
| (1) | The year ended December 31, 2021 includes the application of $11.8 million of Agemo and Gulf Coast security deposits (letter of credit and cash deposits) in revenue. |
| (2) | The year ended December 31, 2021 includes $21.3 million of revenue related to Gulf Coast recognized based on our ability to offset uncollected rent against the interest and principal of certain debt obligations of Omega. |
41
Liquidity and Capital Resources
Sources and Uses
Our primary sources of cash include rental income and interest receipts, existing availability under our Revolving Credit Facility, proceeds from our DRSPP and the 2021 ATM Program, facility sales, and proceeds from mortgage and other investment payoffs. We anticipate that these sources will be adequate to fund our cash flow needs through the next twelve months, which include common stock dividends, debt service payments (including principal and interest), real estate investments (including facility acquisitions, capital improvement programs and other capital expenditures), mortgage and other investment loan advances and normal recurring G&A expenses (primarily consisting of employee payroll and benefits and expenses relating to third parties for legal, consulting and audit services).
Capital Structure
At December 31, 2021, we had total assets of $9.6 billion, total equity of $4.1 billion and total net debt of $5.3 billion, with such debt representing approximately 56.4% of total capitalization.
Debt
At December 31, 2021, the weighted-average annual interest rate of our debt was 4.13%. Additionally, as of December 31, 2021, 100% of our debt with outstanding principal balances has fixed interest payments (when considering the impact of cash flow hedges). As of December 31, 2021, Omega’s debt obligations consisted of the following:
| ● | A $1.45 billion Revolving Credit Facility that bears interest at LIBOR (or in the case of loans denominated in GBP, the Sterling overnight index average reference rate plus an adjustment of 0.1193% per annum) plus an applicable percentage (with a range of 95 to 185 basis points) based on our credit ratings. The Revolving Credit Facility matures on April 30, 2025, subject to Omega’s option to extend such maturity date for two six-month periods. As of December 31, 2021, Omega had no borrowings on the Revolving Credit Facility. |
| ● | A $50.0 million OP Term Loan that bears interest at LIBOR plus an applicable percentage (with a range of 85 to 185 basis points) based on our credit ratings. The interest on the OP Term Loan is effectively fixed at 3.29%, as we have interest rate swaps that effectively hedge the interest payments on this loan. The OP Term Loan matures on April 30, 2025, subject to Omega OP’s option to extend such maturity date for two six-month periods. |
| ● | $4.9 billion of senior unsecured notes with staggered maturity dates in 2023, 2024, 2025, 2026, 2027, 2028, 2029, 2031 and 2033. These notes bear fixed interest rates between 3.25% and 5.25% per annum. |
| ● | $362.1 million of secured borrowings consisting of HUD Mortgages and a term loan. We had $359.8 million of outstanding HUD Mortgages as of December 31, 2021, with weighted average interest rates of 3.01% per annum that mature from 2046 to 2052. |
As of December 31, 2021, we had long-term credit ratings of Baa3 from Moody’s and BBB- from S&P Global and Fitch. Credit ratings impact our ability to access capital and directly impact our cost of capital as well. For example, our Revolving Credit Facility accrues interest and fees at a rate per annum equal to LIBOR plus a margin that depends upon our credit rating. A downgrade in credit ratings by Moody’s and S&P Global may have a negative impact on the interest rates and fees for our Revolving Credit Facility.
Our credit facilities that reference LIBOR contain customary LIBOR replacement language, including, but not limited to, the use of rates based on the secured overnight financing rate.
Certain of our other secured and unsecured borrowings are subject to customary affirmative and negative covenants, including financial covenants. As of December 31, 2021 and 2020, we were in compliance with all affirmative and negative covenants, including financial covenants, for our secured and unsecured borrowings.
42
Equity
At December 31, 2021, we had 239.1 million shares of common stock outstanding and our shares had a market value of $7.1 billion. As of December 31, 2021, we had the following equity programs in place that we can utilize to raise capital:
| ● | The 2021 ATM Program under which shares of common stock having an aggregate gross sales price of up to $1.0 billion may be sold from time to time. The 2021 ATM Program has a forward sale provision that generally allows Omega to lock in a price on the sale of shares of common stock when sold by the forward sellers but defer receiving the net proceeds from such sales until the shares of our common stock are issued at settlement on a later date. We did not utilize the forward provisions under the 2021 ATM Program during 2021. We have $929.9 million of sales remaining under the 2021 ATM Program as of December 31, 2021. |
| ● | We have a DRSPP that allows for the reinvestment of dividends and the optional purchase of our common stock. |
Dividends
As a REIT, we are required to distribute dividends (other than capital gain dividends) to our stockholders in an amount at least equal to (A) the sum of (i) 90% of our “REIT taxable income” (computed without regard to the dividends paid deduction and our net capital gain), and (ii) 90% of the net income (after tax), if any, from foreclosure property, minus (B) the sum of certain items of non-cash income. In addition, if we dispose of any built-in gain asset during a recognition period, we will be required to distribute at least 90% of the built-in gain (after tax), if any, recognized on the disposition of such asset. Such distributions must be paid in the taxable year to which they relate, or in the following taxable year if declared before we timely file our tax return for such year and paid on or before the first regular dividend payment after such declaration. In addition, such distributions are required to be made pro rata, with no preference to any share of stock as compared with other shares of the same class, and with no preference to one class of stock as compared with another class except to the extent that such class is entitled to such a preference. To the extent that we do not distribute all of our net capital gain or do distribute at least 90%, but less than 100% of our “REIT taxable income” as adjusted, we will be subject to tax thereon at regular ordinary and capital gain corporate tax rates.
In 2021, we paid dividends of $637.6 million to our common stockholders.
The Board has declared common stock dividends as set forth below:
|
|
Dividend per |
|||
Record Date |
|
Payment Date |
|
Common Share |
|
February 8, 2021 |
February 16, 2021 |
$ |
0.67 |
||
May 3, 2021 |
May 17, 2021 |
0.67 |
|||
August 2, 2021 |
August 13, 2021 |
0.67 |
|||
November 5, 2021 |
November 15, 2021 |
0.67 |
|||
February 7, 2022 |
February 15, 2022 |
0.67 |
|||
43
Material Cash Requirements
The following table shows our material cash requirements, described below, as of December 31, 2021:
Payments due by period |
|||||||||||||||
|
|
Less than |
|
|
|
More than |
|||||||||
|
Total |
|
1 year |
|
Years 2-3 |
|
Years 4-5 |
|
5 years |
||||||
|
(in thousands) |
||||||||||||||
Debt(1) |
$ |
5,312,081 |
$ |
9,945 |
$ |
766,048 |
$ |
1,067,041 |
$ |
3,469,047 |
|||||
Interest payments on long-term debt |
|
1,416,255 |
|
203,029 |
|
395,235 |
|
320,497 |
|
497,494 |
|||||
Operating lease and other obligations(2) |
|
41,236 |
|
1,998 |
|
4,132 |
|
3,883 |
|
31,223 |
|||||
Total |
$ |
6,769,572 |
$ |
214,972 |
$ |
1,165,415 |
$ |
1,391,421 |
$ |
3,997,764 |
|||||
| (1) | The $5.3 billion of debt outstanding includes: (i) $50 million under the OP Term Loan due April 2025, (ii) $350 million of 4.375% Senior Notes due August 2023, (iii) $400 million of 4.95% Senior Notes due April 2024, (iv) $400 million of 4.50% Senior Notes due January 2025, (v) $600 million of 5.25% Senior Notes due January 2026, (vi) $700 million of 4.5% Senior Notes due April 2027, (vii) $550 million of 4.75% Senior Notes due January 2028, (viii) $500 million of 3.625% Senior Notes due October 2029, (ix) $700 million of 3.375% Senior Notes due February 2031, (x) $700 million of 3.25% Senior Notes due April 2033, (xi) $2.3 million of 3.75% per annum debt held at a consolidated joint venture due February 2022 and (xii) $360 million of HUD debt at a 3.01% weighted average interest rate due between 2046 and 2052. Other than the $50 million outstanding under the OP Term Loan, the $360 million of HUD debt and the $2.3 million of debt held at a consolidated joint venture, Parent is the obligor of all outstanding debt. |
| (2) | In connection with the adoption of Topic 842, we recognized lease liabilities in connection with ground and/or facility leases. Certain operators pay these obligations directly to the landlord. We recognize rental income for ground and/or facility leases where the operator reimburses us, or pays the obligation directly to the landlord on our behalf. |
In addition to the obligations in the table above, as of December 31, 2021, we also had $244.7 million of commitments to fund the construction of new leased and mortgaged facilities, capital improvements and other commitments. Additionally, we have commitments to fund $50.1 million of advancements under existing other investment loans. These commitments are expected to be funded over the next several years and are dependent upon the operators’ election to use the commitments.
Other Arrangements
We own interests in certain unconsolidated joint ventures as described in Note 11 to the Consolidated Financial Statements. Our risk of loss is generally limited to our investment in the joint venture and any outstanding loans receivable. We use derivative instruments to hedge interest rate and foreign currency exchange rate exposure as discussed in Note 15 to the Consolidated Financial Statements.
Cash Flow Summary
The following is our discussion of our consolidated cash flows for the year ended December 31, 2021 as compared to the year ended December 31, 2020. For a discussion of our consolidated cash flows for the year ended December 31, 2020 as compared to the year ended December 31, 2019, see “Item 7 – Management’s Discussion and Analysis of Financial Condition and Results of Operations” of our 2020 Form 10-K.
Cash, cash equivalents and restricted cash totaled $24.4 million as of December 31, 2021, a decrease of $143.1 million as compared to the balance at December 31, 2020. The following is a discussion of changes in cash, cash equivalents and restricted cash due to operating, investing and financing activities, which are presented in our Consolidated Statements of Cash Flows.
Operating Activities – Operating activities generated $722.1 million of net cash flow for the year ended December 31, 2021, as compared to $708.3 million for the same period in 2020, an increase of $13.9 million, which is primarily driven by an increase of $77.8 million of net income, adjusted for non-cash items, due to revenue growth as a result of facility acquisitions and transitions, investments in mortgages and other investments. This increase was partially offset by a $63.9 million change in the net movements of the operating assets and liabilities, primarily driven by the change in receivables driven by operator collectibility issues with Agemo, Guardian and Gulf Coast.
44
Investing Activities – Net cash flow from investing activities was an outflow of $524.2 million for the year ended December 31, 2021, as compared to an outflow of $89.1 million for the same period in 2020. The $435.1 million change in cash used by investing activities related primarily to (i) a $510.2 million increase in real estate acquisitions, primarily related to the acquisition of 24 senior living facilities from Healthpeak in the first quarter of 2021, (ii) $8.0 million increase in investments in unconsolidated joint ventures primarily related to Second Spring II LLC, a new joint venture investment in 2021, (iii) a $33.8 million increase in capital improvements to real estate investments and construction in progress (including $68.0 million related to the purchase of a real estate property located in Washington, D.C. that Omega, in conjunction with Maplewood, plans to redevelop), (iv) a $35.6 million increase in other investments, net of repayments driven by lower repayments in 2021 and (v) a $14.7 million decrease in proceeds from sale of direct financing lease assets and related trust related to Orianna. Offsetting these changes were: (i) a $11.1 million decrease in mortgage placements, net of repayments which is primarily driven by higher repayments in 2021, (ii) $137.7 million increase in proceeds from the sales of real estate investments driven by an attractive real estate market in which Omega elected to sell non-strategic assets, (iii) a $5.1 million decrease in business acquisitions and (iv) a $5.1 million increase in receipts from insurance proceeds.
Financing Activities – Net cash flow from financing activities was an outflow of $341.1 million for the year ended December 31, 2021, as compared to an outflow of $485.5 million for the same period in 2020. The $144.4 million change in cash used in financing activities was primarily related to (i) a $82.8 million change in other long-term borrowings – net which is the result of greater additional long-term borrowings in 2021 (including the issuance of $700 million 3.25% Senior Notes due in 2033) as compared to 2020, partially offset by other long-term debt repayments in 2021 (including pay downs of $350 million on the 4.375% Senior Notes due in 2023, $138.4 million related to the Sterling term loan and $102.5 million on the 2017 Revolving Credit Facility), and (ii) a $122.2 million increase in cash proceeds from the issuance of common stock in 2021, as compared to the same period in 2020 primarily driven by $126.7 million of proceeds from the DRSPP in 2021, offset by (a) a $25.3 million increase in dividends paid primarily resulting from additional share issuances throughout 2020 and 2021 and (b) a $30.8 million increase in payment of financing related costs related to the redemption of $350 million of the 4.375% Senior Notes due 2023 and entering new debt facilities in 2021 such as the Revolving Credit Facility, the OP Term Loan and the 3.25% Senior Notes due 2033.
Supplemental Guarantor Information
Parent has issued approximately $4.9 billion aggregate principal of senior notes outstanding at December 31, 2021 that were registered under the Securities Act of 1933, as amended. The senior notes are guaranteed by Omega OP.
The SEC adopted amendments to Rule 3-10 of Regulation S-X and created Rule 13-01 to simplify disclosure requirements related to certain registered securities, such as our senior notes. As a result of these amendments, registrants are permitted to provide certain alternative financial and non-financial disclosures, to the extent material, in lieu of separate financial statements for subsidiary issuers and guarantors of registered debt securities. Accordingly, separate consolidated financial statements of Omega OP have not been presented. Parent and Omega OP, on a combined basis, have no material assets, liabilities or operations other than financing activities (including borrowings under the senior unsecured revolving and term loan credit facility, Omega OP term loan and the outstanding senior notes) and their investments in non-guarantor subsidiaries.
Omega OP is currently the sole guarantor of our senior notes. The guarantees by Omega OP of our senior notes are full and unconditional and joint and several with respect to the payment of the principal and premium and interest on our senior notes. The guarantees of Omega OP are senior unsecured obligations of Omega OP that rank equal with all existing and future senior debt of Omega OP and are senior to all subordinated debt. However, the guarantees are effectively subordinated to any secured debt of Omega OP. As of December 31, 2021, there were no significant restrictions on the ability of Omega OP to make distributions to Omega.
Critical Accounting Policies and Estimates
The preparation of financial statements in conformity with GAAP in the U.S. requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and the reported amounts of revenues and expenses. Our significant accounting policies are described in Note 2 – Summary of Significant Accounting Policies to the Consolidated Financial Statements. These policies were followed in preparing the Consolidated Financial Statements for all periods presented. Actual results could differ from those estimates.
45
We have identified the following significant accounting policies that we believe are critical accounting policies. These critical accounting policies are those that have the most impact on the reporting of our financial condition and those requiring significant assumptions, judgments and estimates. With respect to these critical accounting policies, we believe the application of assumptions, judgments and estimates is consistently applied and produces financial information that fairly presents the results of operations for all periods presented. The following table presents information about our critical accounting policies, as well as the material assumptions used to develop each estimate:
Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Revenue Recognition |
|
Rental income from our operating leases is generally recognized on a straight-line basis over the lease term when we have determined that the collectibility of substantially all of the lease payments are probable. If we determine that it is not probable that substantially all of the lease payments will be collected, we account for the revenue under the lease on a cash basis. |
We assess the probability of collecting substantially all payments under our leases based on several factors, including, among other things, payment history of the lessee, the financial strength of the lessee and any guarantors, historical operations and operating trends, current and future economic conditions and expectations of performance (which includes known substantial doubt about an operator’s ability to continue as a going concern). If our evaluation of these factors indicates it is probable that we will be unable to collect substantially all rents, we place that operator on a cash basis and limit our rental income to the lesser of lease income on a straight-line basis plus variable rents when they become accruable or cash collected. As a result of placing an operator on a cash basis, we may recognize a charge to rental income for any contractual rent receivable, straight-line rent receivable and lease inducements. |
Real Estate Investment Impairment |
|
Assessing impairment of real property involves subjectivity in determining if indicators of impairment are present and in estimating the future undiscounted cash flows. The estimated future undiscounted cash flows are generally based on the related lease which relates to one or more properties and may include cash flows from the eventual disposition of the asset. In some instances, there may be various potential outcomes for a real estate investment and its potential future cash flows. In these instances, the undiscounted future cash flows used to assess the recoverability are probability-weighted based on management’s best estimates as of the date of evaluation. These estimates can have a significant impact on the undiscounted cash flows. |
We evaluate our real estate investments for impairment indicators at each reporting period, including the evaluation of our assets’ useful lives. The judgment regarding the existence of impairment indicators is based on factors such as, but not limited to, market conditions, operator performance including the current payment status of contractual obligations and expectations of the ability to meet future contractual obligations, legal structure, as well as our intent with respect to holding or disposing of the asset. If indicators of impairment are present, we evaluate the carrying value of the related real estate investments in relation to our estimate of future undiscounted cash flows of the underlying facilities to determine if an impairment charge is necessary. This analysis requires us to use judgment in determining whether indicators of impairment exist, probabilities of potential outcomes and to estimate the expected future undiscounted cash flows or estimated fair values of the facility which impact our assessment of impairment, if any. |
46
Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Asset Acquisitions |
|
We believe that our real estate acquisitions are typically considered asset acquisitions. The assets acquired and liabilities assumed are recognized by allocating the cost of the acquisition, including transaction costs, to the individual assets acquired and liabilities assumed on a relative fair value basis. Tangible assets consist primarily of land, building and site improvements and furniture and equipment. Identifiable intangible assets and liabilities primarily consist of the above or below market component of in-place leases. |
The allocation of the purchase price to the related real estate acquired (tangible assets and intangible assets and liabilities) involves subjectivity as such allocations are based on a relative fair value analysis. In determining the fair values that drive such analysis, we estimate the fair value of each component of the real estate acquired which generally includes land, buildings and site improvements, furniture and equipment, and the above or below market component of in-place leases. Significant assumptions used to determine such fair values include comparable land sales, capitalization rates, discount rates, market rental rates and property operating data, all of which can be impacted by expectations about future market or economic conditions. Our estimates of the values of these components affect the amount of depreciation and amortization we record over the estimated useful life of the property or the term of the lease. |
Allowance for Credit Losses on Mortgages, Other Investments and Direct Financing Leases |
|
For purposes of determining our allowance for credit loss, we pool financial assets that have similar risk characteristics. We aggregate our financial assets by financial instrument type and by internal risk rating. Our internal ratings range between 1 and 7. An internal rating of 1 reflects the lowest likelihood of loss and a 7 reflects the highest likelihood of loss. |
We assess our internal credit ratings on a quarterly basis. Our internal credit ratings consider several factors including the collateral and/or security, the performance of borrowers underlying facilities, if applicable, available credit support (e.g., guarantees), borrowings with third parties, and other ancillary business ventures and real estate operations of the borrower. |
Item 7A – Quantitative and Qualitative Disclosures About Market Risk
We are exposed to various market risks, including the potential loss arising from adverse changes in interest rates and foreign currency exchange rates. We seek to mitigate the effects of fluctuations in interest rates by matching the terms of new investments with new long-term fixed rate borrowings to the extent possible. We also use financial derivative instruments to hedge our interest rate exposure as well as our foreign currency exchange rate exposure. We do not enter into our market risk sensitive financial instruments and related derivative positions (if any) for trading or speculative purposes. The following disclosures discuss potential fluctuations in interest rates and foreign currency exchange rates and are subjective in nature and are dependent on a number of important assumptions, including estimates of future cash flows, risks, discount rates and relevant comparable market information associated with each financial instrument. Readers are cautioned that many of the statements contained in these paragraphs are forward-looking and should be read in conjunction with our disclosures under the heading “Forward-Looking Statements” set forth above. The use of different market assumptions and estimation methodologies may have a material effect on the reported estimated fair value amounts. Accordingly, the estimates presented below are not necessarily indicative of the amounts we would realize in a current market exchange.
47
Interest Rate Risk
We borrow debt at a combination of variable and fixed rates. Movements in interest rates on our variable rate borrowings would change our future earnings and cash flows but not significantly affect the fair value of those instruments. During the year ended December 31, 2021, we incurred interest expense of $1.1 million related to variable rate borrowings outstanding under our Revolving Credit Facility. Assuming no changes in outstanding balances, a 1% increase in interest rates would not have significantly impacted the annual interest expense on our Revolving Credit Facility. Our OP Term Loan bears interest at a variable interest rate, but the entire outstanding principal of $50.0 million was hedged by two notional interest rate swaps at December 31, 2021 that effectively fix the variable portion of the interest rate at 1.84%. Assuming no changes in outstanding balances, a 1% increase in interest rates would have no effect on annual interest expense because of the interest rate swaps.
A change in interest rates will not affect the interest expense associated with our long-term fixed rate borrowings but will affect the fair value of our long-term fixed rate borrowings. The estimated fair value of our total long-term fixed-rate borrowings at December 31, 2021 was approximately $5.6 billion. A one percent increase in interest rates would result in a decrease in the fair value of long-term fixed-rate borrowings by approximately $319.8 million at December 31, 2021.
At December 31, 2021, we have $400 million of forward interest rate swaps outstanding that are recorded at fair value in other assets on our Consolidated Balance Sheets. The forward-starting swaps hedge the interest rate risk associated with interest payments on a forecasted issuance of fixed rate long-term debt.
Foreign Currency Risk
We are exposed to foreign currency risk through our investments in the U.K. Increases or decreases in the value of the British Pound Sterling relative to the U.S. Dollar impact the amount of net income we earn from our investments in the U.K. Based solely on our results for the year ended December 31, 2021, if the applicable exchange rate was to increase or decrease by 10%, our net income from our consolidated U.K.-based investments would increase or decrease, as applicable by $1.0 million.
To hedge a portion of our net investments in the U.K., at December 31, 2021, we have four foreign currency forward contracts with notional amounts totaling £174.0 million, which mature on March 8, 2024.
Item 8 – Financial Statements and Supplementary Data
The consolidated financial statements and the report of Ernst & Young LLP, Independent Registered Public Accounting Firm, on such financial statements are filed as part of this report beginning on page F-1. There have been no retrospective changes to our Consolidated Statements of Operations for any of the quarters within the two most recent fiscal years that are individually or in the aggregate material.
Item 9 – Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
Item 9A – Controls and Procedures
Evaluation of Disclosure Controls and Procedures
In connection with the preparation of our Form 10-K as of and for the year ended December 31, 2021, management evaluated the effectiveness of the design and operation of disclosure controls and procedures of the Company as of December 31, 2021. Based on this evaluation, the Chief Executive Officer and Chief Financial Officer of the Company concluded that the disclosure controls and procedures of the Company were effective at the reasonable assurance level as of December 31, 2021.
48
Management’s Report on Internal Control over Financial Reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting. The Company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with GAAP and includes those policies and procedures that:
| ● | Pertain to the maintenance of records that in reasonable detail accurately and fairly reflect the transactions and dispositions of the assets of the company; |
| ● | Provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and |
| ● | Provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the company’s assets that could have a material effect on the financial statements. |
All internal control systems, no matter how well designed, have inherent limitations and can provide only reasonable, not absolute, assurance that the objectives of the control system are met. Further, the design of a control system must reflect the fact that there are resource constraints, and the benefits of controls must be considered relative to their costs. Because of the inherent limitations in all control systems, no evaluation of controls can provide absolute assurance that all control issues and instances of fraud, if any, within our company have been detected. Therefore, even those systems determined to be effective can provide only reasonable assurance with respect to financial statement preparation and presentation.
In connection with the preparation of this Form 10-K, our management assessed the effectiveness of the Company’s internal control over financial reporting as of December 31, 2021. In making that assessment, our management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission (“COSO”) in Internal Control-Integrated Framework (“2013 framework”). Based on management’s assessment, management believes that, as of December 31, 2021, the Company’s internal control over financial reporting was effective based on those criteria.
The independent registered public accounting firm’s attestation reports regarding the Company’s internal control over financial reporting is included in the 2021 financial statements under the caption entitled Report of Independent Registered Public Accounting Firm and is incorporated herein by reference.
Changes in Internal Control Over Financial Reporting
There were no changes in the Company’s internal control over financial reporting during the quarter ended December 31, 2021 identified in connection with the evaluation of their disclosure controls and procedures described above that have materially affected, or are reasonably likely to materially affect, its internal control over financial reporting.
Item 9B – Other Information
On February 2, 2022, we issued an earnings release reporting our financial and operating results for the fourth quarter and full year ended December 31, 2021. A copy of the earnings release was furnished to the SEC as Exhibit 99.1 to our Current Report on Form 8-K on February 2, 2022. The earnings release inadvertently included an error in the table presenting the tax treatment of 2021 dividends paid to shareholders. Specifically, for all dividends paid in 2021 (on February 16th, May 17th, August 13th and November 15th) the correct percentage of dividends taxable as a return on capital was 4.3802% (rather than 21.4776% stated in the earnings release) and the correct percentage of dividends taxable as a capital gain was 21.4776% (rather than 4.3802% stated in the earnings release). This inadvertent error had no impact on our financial statements or operating results reported in the earnings release. Additionally, this information was correctly included in the 1099 forms provided to shareholders and on our website at www.omegahealthcare.com under the “Investor Relations” tab under “Dividend Taxation.” A corrected earnings release is posted on our website under the “Investors Relations” tab under “Press Releases”.
49
PART III
Item 10 – Directors, Executive Officers of the Registrant and Corporate Governance
The information required by this item is incorporated herein by reference to our Company’s definitive proxy statement for the 2022 Annual Meeting of Stockholders, to be filed with the SEC pursuant to Regulation 14A.
For information regarding executive officers of our Company, see Item 1 – Business – Information about our Executive Officers.
Code of Business Conduct and Ethics
We have adopted a written Code of Business Conduct and Ethics (“Code of Ethics”) that applies to all of our directors and employees, including our chief executive officer, chief financial officer, chief accounting officer and controller. A copy of our Code of Ethics is available on our website at www.omegahealthcare.com. Any amendment to our Code of Ethics or any waiver of our Code of Ethics that is required to be disclosed will be provided on our website at www.omegahealthcare.com promptly following the date of such amendment or waiver.
Item 11 – Executive Compensation
The information required by this item is incorporated herein by reference to our Company’s definitive proxy statement for the 2022 Annual Meeting of Stockholders, to be filed with the SEC pursuant to Regulation 14A.
Item 12 – Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
The information required by this item is incorporated herein by reference to our Company’s definitive proxy statement for the 2022 Annual Meeting of Stockholders, to be filed with the SEC pursuant to Regulation 14A, except as set forth below.
The following table provides information about shares available for future issuance under our equity compensation plans as of December 31, 2021:
Equity Compensation Plan Information
(c) |
||||||||
Number of securities |
||||||||
(a) |
(b) |
remaining available for |
||||||
Number of securities to |
Weighted-average |
future issuance under |
||||||
be issued upon exercise |
exercise price of |
equity compensation plans |
||||||
of outstanding options, |
outstanding options, |
excluding securities |
||||||
Plan category |
|
warrants and rights (1) |
|
warrants and rights (2) |
|
reflected in column (a) (3) |
||
Equity compensation plans approved by security holders |
|
3,125,423 |
$ |
— |
|
3,321,935 |
||
Equity compensation plans not approved by security holders |
|
— |
|
— |
|
— |
||
Total |
|
3,125,423 |
$ |
— |
|
3,321,935 |
||
| (1) | Reflects (i) 272,752 time-based restricted stock units (“RSUs”) and profit interest units (“PIUs”), (ii) 2,222,048 shares related to performance-based RSUs (“PRSUs”) and performance-based PIUs that could be issued if certain performance conditions are achieved and (iii) 630,623 shares in respect of outstanding deferred stock units. |
| (2) | No exercise price is payable with respect to the RSUs and PRSUs. |
| (3) | Reflects (i) 2,838,290 shares of common stock under our 2018 Stock Incentive Plan and (ii) 483,645 shares of common stock under the Omega Healthcare Investors, Inc. Employee Stock Purchase Plan. |
Item 13 – Certain Relationships and Related Transactions, and Director Independence
The information required by this item is incorporated herein by reference to our Company’s definitive proxy statement for the 2022 Annual Meeting of Stockholders, to be filed with the SEC pursuant to Regulation 14A.
Item 14 – Principal Accountant Fees and Services
The information required by this item is incorporated herein by reference to our Company’s definitive proxy statement for the 2022 Annual Meeting of Stockholders, to be filed with the SEC pursuant to Regulation 14A.
50
PART IV
Item 15 – Exhibits and Financial Statement Schedules
(a)(1) Listing of Consolidated Financial Statements
Title of Document |
|
Page |
Reports of Independent Registered Public Accounting Firm (PCAOB ID: |
F-1 |
|
Consolidated Financial Statements of Omega Healthcare Investors, Inc. |
||
Consolidated Balance Sheets as of December 31, 2021 and 2020 |
F-5 |
|
Consolidated Statements of Operations for the three years ended December 31, 2021 |
F-6 |
|
Consolidated Statements of Comprehensive Income for the three years ended December 31, 2021 |
F-7 |
|
Consolidated Statements of Changes in Equity for the three years ended December 31, 2021 |
F-8 |
|
Consolidated Statements of Cash Flows for the three years ended December 31, 2021 |
F-9 |
|
F-10 |
(a)(2) Listing of Financial Statement Schedules. The following consolidated financial statement schedules are included herein:
F-62 |
||
F-63 |
||
F-65 |
All other schedules for which provision is made in the applicable accounting regulation of the Securities and Exchange Commission are not required under the related instructions or are inapplicable or have been omitted because sufficient information has been included in the notes to the Consolidated Financial Statements.
(a)(3) Listing of Exhibits — See “Index to Exhibits” beginning on Page I-1 of this report.
(b) |
Exhibits — See “Index to Exhibits” beginning on Page I-1 of this report. |
(c) |
Financial Statement Schedules — The following consolidated financial statement schedules are included herein: |
Schedule II —Valuation and Qualifying Accounts
Schedule III — Real Estate and Accumulated Depreciation
Schedule IV — Mortgage Loans on Real Estate
Item 16 – Form 10-K Summary
None.
51
Report of Independent Registered Public Accounting Firm
To the Stockholders and the Board of Directors of Omega Healthcare Investors, Inc.
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Omega Healthcare Investors, Inc. (the Company) as of December 31, 2021 and 2020, the related consolidated statements of operations, comprehensive income, changes in equity and cash flows for each of the three years in the period ended December 31, 2021, and the related notes and financial statement schedules listed in the Index at Item 15(a)(2) (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2021 and 2020, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2021, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company's internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) and our report dated February 17, 2022 expressed an unqualified opinion thereon.
Adoption of ASU No. 2016-13
As discussed in Note 2 to the consolidated financial statements, the Company changed its method of accounting for the measurement of credit losses on financial instruments in 2020 due to the adoption of ASU No. 2016-13, Financial Instruments – Credit Losses (Topic 326): Measurement of Credit Losses on Financial Instruments, and the related amendments.
Basis for Opinion
These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matters
The critical audit matters communicated below are matters arising from the current period audit of the financial statements that were communicated or required to be communicated to the audit committee and that: (1) relate to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective or complex judgments. The communication of the critical audit matters does not alter in any way our opinion on the consolidated financial statements, taken as a whole, and we are not, by communicating the critical audit matters below, providing a separate opinion on the critical audit matters or on the accounts or disclosures to which they relate.
F-1
Collectibility of future lease payments |
|
Description of the Matter |
The Company recognized rental income of $924 million during 2021. As described in Note 2 to the consolidated financial statements, the timing and pattern of rental income recognition for operating leases is affected by the Company’s determination as to whether the collectibility of lease payments is probable. Auditing the Company's accounting for rental income is complex due to the judgment involved in the Company’s determination of the collectibility of future lease payments from its operators. The determination involves consideration of the lessee’s payment history and recent payment trends, an assessment of the financial strength of the lessees and guarantors, where applicable, future contractual rents, historical and projected operating results of the lessees in such properties, and the timing of expected payments. |
How We Addressed the Matter in Our Audit |
We obtained an understanding, evaluated the design and tested the operating effectiveness of the Company's controls over the recognition of rental income, including controls over management’s assessment of the collectibility of future lease payments. For example, we tested controls over management’s consideration of the factors used in assessing collectibility and controls over the completeness and accuracy of the data used in management’s analyses. To test the rental income recognized, we performed audit procedures that included, among others, evaluating the collectibility of lease payments. For example, we assessed the operators’ historical operating results in the properties, the financial condition of the operators and payment trends for a sample of operators. We also considered whether other information obtained throughout the course of our audit procedures corroborated or contradicted management’s analysis. In addition, we tested the completeness and accuracy of the data that was used in management’s analyses. |
Accounting for acquisitions |
|
Description of the Matter |
As described in Note 2 to the financial statements, the Company invested $662.6 million in asset acquisitions, including the acquisition of the Healthpeak Properties, Inc. portfolio for $511.3 million. Auditing the Company's accounting for its acquisitions was complex due to the significant estimation uncertainty in the Company’s determination of the fair value of the acquired assets and liabilities, including the acquired properties and assumed lease. The significant estimation uncertainty was primarily due to the sensitivity of the respective fair values to the underlying significant assumptions utilized in the measurement of the fair value of the acquired properties and lease. The Company used discounted cash flow analyses, market comparable data, and replacement cost data, to estimate the fair value of the acquired properties and assumed lease. The significant assumptions used to estimate the fair value of the acquired properties and assumed lease included lease coverage ratios, lease yields, market rents, land values per acre, discount rates, and replacement costs of furniture, fixtures, and equipment. Certain of these significant assumptions include consideration of future economic and market conditions. |
F-2
How We Addressed the Matter in Our Audit |
We obtained an understanding, evaluated the design, and tested the operating effectiveness of the controls over the Company’s accounting for acquisitions. For example, we tested controls over the measurement of the acquired properties and assumed leases, including management’s review of the appropriateness of the valuation methodology and assumptions used in the valuation models. To test the estimated fair value of the acquired properties and assumed lease, we involved our valuation specialists and performed procedures including, among others, evaluating the Company’s valuation methodology and testing the significant assumptions. For example, we compared the significant assumptions used to independent third-party data and the Company’s recent lease and acquisition transactions. Additionally, we tested the completeness and accuracy of the underlying data supporting the significant assumptions and estimates including through comparison to the related lease agreements. |
/s/
We have served as the Company’s auditor since 1992.
February 17, 2022
F-3
Report of Independent Registered Public Accounting Firm
To the Stockholders and Board of Directors of Omega Healthcare Investors, Inc.
Opinion on Internal Control over Financial Reporting
We have audited Omega Healthcare Investors, Inc.’s internal control over financial reporting as of December 31, 2021, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the COSO criteria). In our opinion, Omega Healthcare Investors, Inc. (the Company) maintained, in all material respects, effective internal control over financial reporting as of December 31, 2021, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the consolidated balance sheets of Omega Healthcare Investors, Inc. as of December 31, 2021 and 2020, the related consolidated statements of operations, comprehensive income, changes in equity and cash flows for each of the three years in the period ended December 31, 2021, and the related notes and financial statement schedules listed in the Index at Item 15(a)(2) and our report dated February 17, 2022 expressed an unqualified opinion thereon.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects.
Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control Over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ Ernst & Young LLP
Baltimore, Maryland
February 17, 2022
F-4
OMEGA HEALTHCARE INVESTORS, INC.
CONSOLIDATED BALANCE SHEETS
(in thousands, except per share amounts)
December 31, |
||||||
|
2021 |
|
2020 |
|||
ASSETS |
||||||
Real estate assets |
|
|
|
|||
Buildings and improvements |
$ |
|
|
$ |
|
|
Land |
|
|
||||
Furniture and equipment |
|
|
||||
Construction in progress |
|
|
||||
Total real estate assets |
|
|
||||
Less accumulated depreciation |
|
( |
|
|
( |
|
Real estate assets – net |
|
|
|
|
|
|
Investments in direct financing leases – net |
|
|
|
|
|
|
Mortgage notes receivable – net |
|
|
|
|
|
|
|
|
|||||
Other investments – net |
|
|
|
|
|
|
Investments in unconsolidated joint ventures |
|
|
|
|
|
|
Assets held for sale |
|
|
|
|
|
|
Total investments |
|
|
|
|
|
|
Cash and cash equivalents |
|
|
|
|
|
|
Restricted cash |
|
|
|
|
|
|
Contractual receivables – net |
|
|
|
|
|
|
Other receivables and lease inducements |
|
|
||||
Goodwill |
|
|
|
|
|
|
Other assets |
|
|
|
|
|
|
Total assets |
$ |
|
|
$ |
|
|
LIABILITIES AND EQUITY |
|
|
|
|
|
|
Revolving credit facility |
$ |
— |
|
$ |
|
|
Secured borrowings |
|
|
|
|
|
|
Senior notes and other unsecured borrowings – net |
|
|
|
|
|
|
Accrued expenses and other liabilities |
|
|
|
|
|
|
Deferred income taxes |
|
|
|
|
|
|
Total liabilities |
|
|
|
|
|
|
Equity: |
|
|
|
|
||
Preferred stock $ |
||||||
Common stock $ |
|
|
|
|
||
Additional paid-in capital |
|
|
|
|
||
Cumulative net earnings |
|
|
|
|
||
Cumulative dividends paid |
|
( |
|
( |
||
Accumulated other comprehensive loss |
|
( |
|
( |
||
Total stockholders’ equity |
|
|
|
|
||
Noncontrolling interest |
|
|
|
|
||
Total equity |
|
|
|
|
||
Total liabilities and equity |
$ |
|
|
$ |
|
|
See accompanying notes.
F-5
OMEGA HEALTHCARE INVESTORS, INC.
CONSOLIDATED STATEMENTS OF OPERATIONS
(in thousands, except per share amounts)
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
|
2019 |
||||
Revenues |
|||||||||
Rental income |
$ |
|
$ |
|
$ |
|
|||
Income from direct financing leases |
|
|
|
|
|
|
|||
Mortgage interest income |
|
|
|
|
|
|
|||
Other investment income |
|
|
|
|
|
|
|||
Miscellaneous income |
|
|
|
|
|
|
|||
Total revenues |
|
|
|
|
|
|
|
||
Expenses |
|
|
|
|
|
|
|
||
Depreciation and amortization |
|
|
|
|
|
|
|||
General and administrative |
|
|
|
|
|
|
|||
Real estate taxes |
|
|
|
||||||
Acquisition, merger and transition related costs |
|
|
|
|
|
|
|||
Impairment on real estate properties |
|
|
|
|
|
|
|||
(Recovery) impairment on direct financing leases |
|
( |
|
( |
|
|
|||
Provision for credit losses |
|
|
|
|
|
— |
|||
Interest expense |
|
|
|
|
|
|
|||
Total expenses |
|
|
|
|
|
|
|
||
Other income (expense) |
|
|
|
|
|
|
|
||
Other (expense) income – net |
|
( |
|
( |
|
|
|||
Loss on debt extinguishment |
|
( |
|
( |
|
— |
|||
Gain on assets sold – net |
|
|
|
||||||
Total other income |
|
|
|
||||||
Income before income tax expense and income from unconsolidated joint ventures |
|
|
|
|
|
|
|
||
Income tax expense |
|
( |
|
( |
|
( |
|||
Income from unconsolidated joint ventures |
|
|
|
|
|
|
|||
Net income |
|
|
|
|
|
|
|
||
Net income attributable to noncontrolling interest |
|
( |
|
( |
|
( |
|||
Net income available to common stockholders |
$ |
|
$ |
|
|
$ |
|
||
Earnings per common share available to common stockholders: |
|
|
|
|
|
|
|
||
Basic: |
|
|
|
|
|
||||
Net income available to common stockholders |
$ |
|
$ |
|
$ |
|
|||
Diluted: |
|
|
|
|
|
|
|||
Net income |
$ |
|
$ |
|
$ |
|
|||
See accompanying notes.
F-6
OMEGA HEALTHCARE INVESTORS, INC.
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME
(in thousands)
|
Year Ended December 31, |
||||||||
|
2021 |
|
2020 |
|
2019 |
||||
Net income |
$ |
|
$ |
|
$ |
|
|||
Other comprehensive income (loss): |
|
|
|
|
|
|
|||
Foreign currency translation |
|
( |
|
|
|
|
|||
Cash flow hedges |
|
|
|
|
|
( |
|||
Total other comprehensive income |
|
|
|
|
|
|
|||
Comprehensive income |
|
|
|
|
|
|
|||
Comprehensive income attributable to noncontrolling interest |
|
( |
|
( |
|
( |
|||
Comprehensive income attributable to common stockholders |
$ |
|
$ |
|
$ |
|
|||
See accompanying notes.
F-7
OMEGA HEALTHCARE INVESTORS, INC.
CONSOLIDATED STATEMENTS OF CHANGES IN EQUITY
(in thousands, except per share amounts)
Accumulated |
|
|||||||||||||||||||||||
Common |
Additional |
Cumulative |
Other |
Total |
|
|||||||||||||||||||
Stock |
Paid‑in |
Net |
Cumulative |
Comprehensive |
Stockholders’ |
Noncontrolling |
Total |
|||||||||||||||||
|
Par Value |
|
Capital |
|
Earnings |
|
Dividends |
|
Loss (Income) |
|
Equity |
|
Interest |
|
Equity |
|||||||||
Balance at December 31, 2018 |
$ |
|
$ |
|
$ |
|
$ |
( |
$ |
( |
$ |
|
$ |
|
$ |
|
||||||||
Cumulative effect of accounting change (see Note 2) |
— |
— |
( |
— |
— |
( |
( |
( |
||||||||||||||||
Stock related compensation |
|
— |
|
|
— |
— |
— |
|
|
|
— |
|
|
|||||||||||
Issuance of common stock |
|
|
|
|
|
— |
|
— |
|
— |
|
|
|
— |
|
|
||||||||
Common dividends declared ($ |
|
— |
— |
— |
( |
— |
|
( |
|
— |
|
( |
||||||||||||
Vesting/exercising of OP units |
— |
( |
— |
— |
— |
( |
|
— |
||||||||||||||||
Conversion and redemption of Omega OP Units to common stock |
|
|
|
|
— |
|
— |
|
— |
|
|
|
( |
|
— |
|||||||||
Omega OP Units distributions |
|
— |
|
— |
|
— |
|
— |
|
— |
|
— |
|
( |
|
( |
||||||||
Noncontrolling interest - consolidated joint venture |
|
— |
— |
— |
— |
— |
|
— |
|
|
|
|
||||||||||||
Other comprehensive income (loss) |
|
— |
|
— |
|
— |
|
— |
|
|
|
|
|
( |
|
|
||||||||
Net income |
|
— |
|
— |
|
|
|
— |
|
— |
|
|
|
|
|
|
||||||||
Balance at December 31, 2019 |
|
|
|
( |
( |
|
|
|
||||||||||||||||
Cumulative effect of accounting change (see Note 2) |
— |
— |
( |
— |
— |
( |
( |
( |
||||||||||||||||
Balance at January 1, 2020 |
|
|
|
|
|
|
|
( |
|
( |
|
|
|
|
|
|
||||||||
Stock related compensation |
|
— |
|
— |
— |
— |
|
|
|
— |
|
|
||||||||||||
Issuance of common stock |
|
|
|
— |
— |
— |
|
|
|
— |
|
|
||||||||||||
Common dividends declared ($ |
— |
— |
— |
( |
— |
( |
— |
( |
||||||||||||||||
Vesting/exercising of OP units |
— |
( |
— |
— |
— |
( |
|
— |
||||||||||||||||
Conversion and redemption of Omega OP Units to common stock |
|
|
|
— |
— |
— |
|
|
|
( |
|
— |
||||||||||||
Omega OP Units distributions |
|
— |
— |
— |
— |
— |
|
— |
|
( |
|
( |
||||||||||||
Other comprehensive income |
|
— |
— |
— |
— |
|
|
|
|
|
|
|
||||||||||||
Net income |
|
— |
— |
|
— |
— |
|
|
|
|
|
|
||||||||||||
Balance at December 31, 2020 |
|
|
|
( |
( |
|
|
|
||||||||||||||||
Stock related compensation |
— |
|
— |
— |
— |
|
— |
|
||||||||||||||||
Issuance of common stock |
|
|
— |
— |
— |
|
— |
|
||||||||||||||||
Common dividends declared ($ |
— |
— |
— |
( |
— |
( |
— |
( |
||||||||||||||||
Vesting/exercising of OP units |
— |
( |
— |
— |
— |
( |
|
— |
||||||||||||||||
Conversion and redemption of Omega OP Units to common stock |
|
|
— |
— |
— |
|
( |
( |
||||||||||||||||
Omega OP Units distributions |
— |
— |
— |
— |
— |
— |
( |
( |
||||||||||||||||
Other comprehensive income |
— |
— |
— |
— |
|
|
|
|
||||||||||||||||
Net income |
— |
— |
|
— |
— |
|
|
|
||||||||||||||||
Balance at December 31, 2021 |
$ |
|
$ |
|
$ |
|
$ |
( |
$ |
( |
$ |
|
$ |
|
$ |
|
||||||||
See accompanying notes.
F-8
OMEGA HEALTHCARE INVESTORS, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands)
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
|
2019 |
||||
Cash flows from operating activities |
|
|
|
|
|
|
|||
Net income |
$ |
|
$ |
|
$ |
|
|||
Adjustment to reconcile net income to net cash provided by operating activities: |
|
|
|
|
|
||||
Depreciation and amortization |
|
|
|
|
|
||||
Impairment on real estate properties |
|
|
|
|
|
||||
(Recovery) impairment on direct financing leases |
( |
|
( |
|
|
||||
Provision for rental income |
|
|
|
|
|
||||
Provision for credit losses |
|
|
|
|
— |
||||
Amortization of deferred financing costs and loss on debt extinguishment |
|
|
|
|
|
||||
Accretion of direct financing leases |
|
|
|
|
|
||||
Stock-based compensation expense |
|
|
|
|
|
||||
Gain on assets sold – net |
( |
|
( |
|
( |
||||
Amortization of acquired in-place leases – net |
( |
|
( |
|
( |
||||
Effective yield payable (receivable) on mortgage notes |
|
|
( |
|
( |
||||
Interest paid-in-kind |
( |
( |
( |
||||||
(Income) loss from unconsolidated joint ventures |
( |
( |
|
||||||
Change in operating assets and liabilities – net: |
|
|
|
|
|||||
Contractual receivables |
( |
|
|
|
( |
||||
Straight-line rent receivables |
( |
|
( |
|
( |
||||
Lease inducements |
( |
|
( |
|
( |
||||
Other operating assets and liabilities |
( |
|
|
|
( |
||||
Net cash provided by operating activities |
|
|
|
|
|
||||
Cash flows from investing activities |
|
|
|
|
|
||||
Acquisition of a business, net of cash acquired |
— |
|
( |
|
( |
||||
Acquisition of real estate |
( |
|
( |
|
( |
||||
Acquisition deposit - net |
( |
|
( |
|
— |
||||
Net proceeds from sale of real estate investments |
|
|
|
|
|
||||
Investments in construction in progress |
( |
|
( |
|
( |
||||
Proceeds from sale of direct financing lease and related trust |
|
|
|
||||||
Placement of mortgage loans |
( |
|
( |
|
( |
||||
Collection of mortgage principal |
|
|
|
|
|
||||
Investments in unconsolidated joint ventures |
( |
( |
( |
||||||
Distributions from unconsolidated joint ventures in excess of earnings |
|
|
|
|
|
||||
Capital improvements to real estate investments |
( |
|
( |
|
( |
||||
Receipts from insurance proceeds |
|
|
|
|
|
||||
Investments in other investments |
( |
|
( |
|
( |
||||
Proceeds from other investments |
|
|
|
|
|
||||
Net cash used in investing activities |
( |
|
( |
|
( |
||||
Cash flows from financing activities |
|
|
|
|
|
||||
Proceeds from long-term borrowings |
|
|
|
|
|
||||
Payments of long-term borrowings |
( |
|
( |
|
( |
||||
Payments of financing related costs |
( |
|
( |
|
( |
||||
Net proceeds from issuance of common stock |
|
|
|
|
|
||||
Dividends paid |
( |
|
( |
|
( |
||||
Noncontrolling members’ contributions to consolidated joint venture |
— |
— |
|
||||||
Redemption of Omega OP Units |
( |
|
— |
|
— |
||||
Distributions to Omega OP Unit Holders |
( |
|
( |
|
( |
||||
Net cash used in financing activities |
( |
|
( |
|
( |
||||
Effect of foreign currency translation on cash, cash equivalents and restricted cash |
|
|
|
|
|
||||
(Decrease) increase in cash, cash equivalents and restricted cash |
( |
|
|
|
|
||||
Cash, cash equivalents and restricted cash at beginning of period |
|
|
|
|
|
||||
Cash, cash equivalents and restricted cash at end of period |
$ |
|
$ |
|
$ |
|
|||
See accompanying notes.
F-9
NOTE 1 - ORGANIZATION
Omega Healthcare Investors, Inc. (“Parent”), is a Maryland corporation that, together with its consolidated subsidiaries (collectively, “Omega”, the “Company”, “we”, “our”, “us”) invests in healthcare-related real estate properties located in the United States (“U.S.”) and the United Kingdom (“U.K.”). Our core business is to provide financing and capital to the long-term healthcare industry with a particular focus on skilled nursing facilities (“SNFs”), assisted living facilities (“ALFs”), and to a lesser extent, independent living facilities (“ILFs”), rehabilitation and acute care facilities (“specialty facilities”) and medical office buildings (“MOBs”). Our core portfolio consists of our long-term “triple-net” leases and mortgage loans with healthcare operating companies and affiliates (collectively, our “operators”). In addition to our core investments, we selectively make loans to operators for working capital and capital expenditures. From time to time, we also acquire equity interests in joint ventures or entities that support the long-term healthcare industry and our operators.
Omega has elected to be taxed as a real estate investment trust (“REIT”) for federal income tax purposes and is structured as an umbrella partnership REIT (“UPREIT”) under which all of Omega's assets are owned directly or indirectly by, and all of Omega's operations are conducted directly or indirectly through, its operating partnership subsidiary, OHI Healthcare Properties Limited Partnership (collectively with subsidiaries, “Omega OP”). Omega has exclusive control over Omega OP’s day-to-day management pursuant to the partnership agreement governing Omega OP. As of December 31, 2021, Parent owned approximately
NOTE 2 – SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Accounting Estimates
The preparation of financial statements in conformity with U.S. generally accepted accounting principles (“GAAP”) requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities, the disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates.
Consolidation
Omega’s consolidated financial statements include the accounts of (i) Parent, (ii) Omega OP, (iii) all direct and indirect wholly-owned subsidiaries of Omega and (iv) other entities in which Omega or Omega OP has a majority voting interest and control. All intercompany transactions and balances have been eliminated in consolidation, and Omega’s net earnings are reduced by the portion of net earnings attributable to noncontrolling interests.
GAAP requires us to identify entities for which control is achieved through means other than voting rights and to determine which business enterprise, if any, is the primary beneficiary of variable interest entities (“VIEs”). A VIE is broadly defined as an entity with one or more of the following characteristics: (a) the total equity investment at risk is insufficient to finance the entity’s activities without additional subordinated financial support; (b) as a group, the holders of the equity investment at risk lack (i) the ability to make decisions about the entity’s activities through voting or similar rights, (ii) the obligation to absorb the expected losses of the entity, or (iii) the right to receive the expected residual returns of the entity; or (c) the equity investors have voting rights that are not proportional to their economic interests, and substantially all of the entity’s activities either involve, or are conducted on behalf of, an investor that has disproportionately few voting rights. We may change our original assessment of a VIE upon subsequent events such as the modification of contractual arrangements that affects the characteristics or adequacy of the entity’s equity investments at risk and the disposition of all or a portion of an interest held by the primary beneficiary.
Our variable interests in VIEs may be in the form of equity ownership, leases, guarantees and/or loans with our operators. We analyze our agreements and investments to determine whether our operators or unconsolidated joint ventures are VIEs and, if so, whether we are the primary beneficiary.
F-10
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
We consolidate a VIE when we determine that we are its primary beneficiary. We identify the primary beneficiary of a VIE as the enterprise that has both: (i) the power to direct the activities of the VIE that most significantly impact the entity’s economic performance; and (ii) the obligation to absorb losses or the right to receive benefits of the VIE that could be significant to the entity. Factors considered in determining whether we are the primary beneficiary of an entity include: (i) our voting rights, if any; (ii) our involvement in day-to-day capital and operating decisions; (iii) our risk and reward sharing; (iv) the financial condition of the operator or joint venture and (iv) our representation on the VIE’s board of directors. We perform this analysis on an ongoing basis. As of December 31, 2021 and 2020 we did not have any VIEs that we consolidated.
Revenue Recognition
Rental Income
Substantially all of our operating leases contain provisions for specified annual increases over the rents of the prior year and are generally computed in one of three methods depending on the specific provisions of each lease as follows: (i) a specific annual increase over the prior year’s rent, generally between
We assess the probability of collecting substantially all payments due under our leases on several factors, including, among other things, payment history, the financial strength of the lessee and/or borrower and any guarantors, historical operations and operating trends, current and future economic conditions, and expectations of performance (which includes known substantial doubt about an operator’s ability to continue as a going concern). If our evaluation of these factors indicates it is probable that we will be unable to collect substantially all rents, we recognize a charge to rental income and limit our rental income to the lesser of lease income on a straight-line basis plus variable rents when they become accruable or cash collected. Provisions for uncollectible lease payments are recognized as a direct reduction to rental income. If we change our conclusion regarding the probability of collecting rent payments required by a lessee, we may recognize an adjustment to rental income in the period we make a change to our prior conclusion, potentially resulting in increased volatility of rental income.
Our leased real estate properties are leased under provisions of single or master leases with initial terms typically ranging from
Under the terms of the leases, the lessee is responsible for all maintenance, repairs, taxes and insurance on the leased properties. Certain of our operating leases require the operators to reimburse us for property taxes and other expenditures that are not considered components of the lease and therefore no consideration is allocated to them as they do not result in the transfer of a good or service to the operators. We have determined that all of our leases qualify for the practical expedient to not separate the lease and non-lease components because (i) the lease components are operating leases and (ii) the timing and pattern of recognition of the non-lease components are the same as the lease components. We apply Accounting Standards Codification (“ASC”) 842, Leases (“Topic 842”) to the combined component.
Certain operators are obligated to pay directly their obligations under their leases for real estate taxes, insurance and certain other expenses. These obligations, which have been assumed by the tenants under the terms of their respective leases, are not reflected in our consolidated financial statements. To the extent any tenant responsible for these obligations under their respective lease defaults on its lease or if it is deemed probable that the tenant will fail to pay for such costs, we would record a liability for such obligation.
We have elected to exclude sales and other similar taxes from the measurement of lease revenue and expense.
F-11
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Mortgage Interest Income and Other Investment Income
Mortgage interest income and other investment income is recognized as earned over the terms of the related mortgage notes or other investment. Interest income is recorded on an accrual basis to the extent that such amounts are expected to be collected using the effective interest method. In applying the effective interest method, the effective yield on a loan is determined based on its contractual payment terms, adjusted for prepayment terms.
Direct Financing Lease Income
As of December 31, 2021, we have
Fair Value Measurement
The Company measures and discloses the fair value of nonfinancial and financial assets and liabilities utilizing a hierarchy of valuation techniques based on whether the inputs to a fair value measurement are considered to be observable or unobservable in a marketplace. Observable inputs reflect market data obtained from independent sources, while unobservable inputs reflect the Company’s market assumptions. This hierarchy requires the use of observable market data when available. These inputs have created the following fair value hierarchy:
| ● | Level 1 - quoted prices for identical instruments in active markets; |
| ● | Level 2 - quoted prices for similar instruments in active markets; quoted prices for identical or similar instruments in markets that are not active; and model-derived valuations in which significant inputs and significant value drivers are observable in active markets; and |
| ● | Level 3 - fair value measurements derived from valuation techniques in which one or more significant inputs or significant value drivers are unobservable. |
The Company measures fair value using a set of standardized procedures that are outlined herein for all assets and liabilities which are required to be measured at fair value. When available, the Company utilizes quoted market prices from an independent third-party source to determine fair value and classifies such items in Level 1. In some instances where a market price is available, but the instrument is in an inactive or over-the-counter market, the Company consistently applies the dealer (market maker) pricing estimate and classifies such items in Level 2.
If quoted market prices or inputs are not available, fair value measurements are based upon valuation models that utilize current market or independently sourced market inputs, such as interest rates, option volatilities, credit spreads and/or market capitalization rates. Items valued using such internally-generated valuation techniques are classified according to the lowest level input that is significant to the fair value measurement. As a result, these items could be classified in either Level 2 or Level 3 even though there may be some significant inputs that are readily observable. Internal fair value models and techniques used by the Company include discounted cash flow and Monte Carlo valuation models.
F-12
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Risks and Uncertainties including COVID-19
The Company is subject to certain risks and uncertainties affecting the healthcare industry, including those stemming from the novel coronavirus (“COVID-19”) global pandemic, which has disproportionately impacted the senior care sector, as well as, those stemming from healthcare legislation and changing regulation by federal, state and local governments. Additionally, we are subject to risks and uncertainties as a result of changes affecting operators of nursing home facilities due to the actions of governmental agencies and insurers to limit the rising cost of healthcare services.
Real Estate Acquisitions
Upon acquisition of real estate properties, we evaluate the acquisition to determine if it is a business combination or an asset acquisition. Our real estate acquisitions are generally accounted for as asset acquisitions as substantially all of the fair value of the gross assets acquired is concentrated in a single identifiable asset or group of similar identifiable assets.
If the acquisition is determined to be an asset acquisition, the Company records the purchase price and other related costs incurred to the acquired tangible assets and identified intangible assets and liabilities on a relative fair value basis. In addition, costs incurred for asset acquisitions including transaction costs, are capitalized.
If the acquisition is determined to be a business combination, we record the purchase of properties to net tangible and identified intangible assets acquired and liabilities assumed at fair value. Goodwill is measured as the excess of the fair value of the consideration transferred over the fair value of the identifiable net assets. Transaction costs are expensed as incurred as part of a business combination.
In making estimates of fair value for purposes of recording asset acquisitions and business combinations, we utilize a number of sources, including independent appraisals that may be obtained in connection with the acquisition or financing of the respective property and other market data. The Company determines the fair value of acquired assets and liabilities as follows:
| ● | Land is determined based on third-party appraisals which typically include market comparables. |
| ● | Buildings and site improvements acquired are valued using a combination of discounted cash flow projections that assume certain future revenues and costs and consider capitalization and discount rates using current market conditions as well as the residual approach. |
| ● | Furniture and fixtures are determined based on third-party appraisals which typically utilize a replacement cost approach. |
| ● | Mortgages and other investments are valued using a discounted cash flow analysis, using interest rates being offered for similar loans to borrowers with similar credit ratings. |
| ● | Investments in joint ventures are valued based on the fair value of the joint ventures’ assets and liabilities. Differences, if any, between the Company’s basis and the joint venture’s basis are generally amortized over the lives of the related assets and liabilities, and such amortization is included in the Company’s share of earnings (losses) of the joint venture. |
| ● | Intangible assets and liabilities acquired are valued using a combination of discounted cash flow projections as well as other valuation techniques based on current market conditions for the intangible asset or liability being acquired. When evaluating below market leases we consider extension options controlled by the lessee in our evaluation. |
| ● | Other assets acquired and liabilities assumed are typically valued at stated amounts, which approximate fair value on the date of the acquisition. |
| ● | Assumed debt balances are valued by discounting the remaining contractual cash flows using a current market rate of interest. |
F-13
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
| ● | Noncontrolling interests are valued using a stock price on the acquisition date. |
Real Estate Properties
Real estate properties are carried at initial recorded value less accumulated depreciation. The costs of significant improvements, renovations and replacements, including interest are capitalized. Our interest expense reflected in the Consolidated Statements of Operations has been reduced by the amounts capitalized. For the years ended December 31, 2021, 2020 and 2019, we capitalized $
Depreciation is computed on a
Management evaluates our real estate properties for impairment indicators at each reporting period, including the evaluation of our assets’ useful lives. The judgment regarding the existence of impairment indicators is based on factors such as, but not limited to, market conditions, operator performance including the current payment status of contractual obligations and expectations of the ability to meet future contractual obligations, legal structure, as well as our intent with respect to holding or disposing of the asset. If indicators of impairment are present, management evaluates the carrying value of the related real estate investments in relation to management’s estimate of future undiscounted cash flows of the underlying facilities. The estimated future undiscounted cash flows are generally based on the related lease which relates to one or more properties and may include cash flows from the eventual disposition of the asset. In some instances, there may be various potential outcomes for a real estate investment and its potential future cash flows. In these instances, the undiscounted future cash flows used to assess the recoverability of the assets are probability-weighted based on management’s best estimates as of the date of evaluation. Impairment losses related to long-lived assets are recognized when expected future undiscounted cash flows based on our intended use of the property are determined to be less than the carrying values of the assets. An adjustment is made to the net carrying value of the real estate investments for the excess of carrying value over fair value. The fair value of the real estate investment is determined based on current market conditions and considers matters such as rental rates and occupancies for comparable properties, recent sales data for comparable properties, and, where applicable, contracts or the results of negotiations with purchasers or prospective purchasers. Additionally, our evaluation of fair value may consider valuing the property as a nursing home or other healthcare facility as well as alternative uses. All impairments are taken as a period cost at that time, and depreciation is adjusted going forward to reflect the new value assigned to the asset. Management’s impairment evaluation process, and when applicable, impairment calculations involve estimation of the future cash flows from management’s intended use of the property as well as the fair value of the property. Changes in the facts and circumstances that drive management’s assumptions may result in an impairment to our assets in a future period that could be material to our results of operations.
Assets Held for Sale
We consider properties to be assets held for sale when (1) management commits to a plan to sell the property; (2) it is unlikely that the disposal plan will be significantly modified or discontinued; (3) the property is available for immediate sale in its present condition; (4) actions required to complete the sale of the property have been initiated; (5) sale of the property is probable and we expect the completed sale will occur within one year; and (6) the property is actively being marketed for sale at a price that is reasonable given our estimate of current market value. Upon designation of a property as an asset held for sale, we record the property’s value at the lower of its carrying value or its estimated fair value, less estimated costs to sell, and we cease depreciation.
Real Estate Sales
We recognize gains related to the sale of real estate when we transfer control of the property and when it is probable that we will collect substantially all of the related consideration.
F-14
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Lessee Accounting
Omega leases real estate (corporate headquarters and certain other facilities), office equipment and is party to certain ground leases on our owned facilities. We determine if an arrangement is or contains a lease at inception. Leases are classified as either finance or operating at inception of the lease. Short-term leases, defined as leases with an initial term of 12 months or less that do not contain a purchase option, are not recorded on the balance sheet. Lease expense for short-term leases is recognized on a straight-line basis over the lease term. As of December 31, 2021 and 2020, all of the leases where we are the lessee were classified as operating leases.
We have leases that contain both lease and non-lease components and have elected, as an accounting policy, to not separate lease components and non-lease components. Operating and finance lease right of use ("ROU") assets and liabilities are recognized at the commencement date based on the present value of lease payments over the lease term. Our ROU assets and lease liabilities are included in other assets and accrued expenses and other liabilities, respectively, on our Consolidated Balance Sheets. The lease liability is calculated as the present value of the remaining minimum rental payments for existing leases using either the rate implicit in the lease or, if none exists, the Company's incremental borrowing rate, as the discount rate. Certain leases have options to extend, terminate or purchase the asset and have been considered in our analysis of the lease term and the measurement of the right-of-use assets and lease liabilities.
On a quarterly basis, we remeasure our lease liabilities at the present value of the future lease payments using the discount rate determined at lease commencement. Rental expense from operating leases is generally recognized on a straight-line basis over the lease term. Lease expense derived from our operating leases is recorded in general and administrative in our Consolidated Statements of Operations. We do not include in our measurement of our lease liability certain variable payments, including changes in an index until the specific events that trigger the variable payments have occurred.
We record on a straight-line basis rental income and ground lease expense for those assets we lease and are reimbursed by our operators and/or are paid for directly by our operators.
In-Place Leases
In-place lease assets and liabilities result when we assume a lease as part of an asset acquisition or business combination. The fair value of in-place leases consists of the following components, as applicable (1) the estimated cost to replace the leases and (2) the above or below market cash flow of the leases, determined by comparing the projected cash flows of the leases in place at the time of acquisition to projected cash flows of comparable market-rate leases.
Above market leases, net of accumulated amortization, are included in other assets on our Consolidated Balance Sheets. Below market leases, net of accumulated amortization, are included in accrued expenses and other liabilities on our Consolidated Balance Sheets. The net amortization related to the above and below market leases is included in our Consolidated Statements of Operations as an adjustment to rental income over the estimated remaining term of the underlying leases. Should a tenant terminate the lease, the unamortized portion of the lease intangible is recognized immediately as an adjustment to rental income.
Allowance for Credit Losses
The allowance for credit losses reflects our current estimate of the potential credit losses on our mortgage notes, other investment loans, and our investment in direct financing leases and is recorded as a valuation account as a direct offset against these financial instruments on our Consolidated Balance Sheets. Expected credit losses inherent in non-cancelable unfunded loan commitments are accounted for as separate liabilities included in accrued expenses and other liabilities on the Consolidated Balance Sheets. The Company has elected to not measure an allowance for credit losses on accrued interest receivables related to all of its mortgage notes and other investment loans because we write off uncollectible accrued interest receivable in a timely manner pursuant to our non-accrual policy, described below. Changes to the allowance for credit losses on loans resulting from quarterly evaluations are recorded through provision for credit losses on the Consolidated Statements of Operations.
F-15
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
We assess the creditworthiness of our borrowers on a quarterly basis. For purposes of determining our allowance for credit loss, we pool financial assets that have similar risk characteristics. We aggregate our financial assets by financial instrument type (i.e. mortgage, other investment, etc.) and by internal risk rating. Our internal credit ratings consider several factors including the collateral and/or security, the performance of borrowers underlying facilities, if applicable, available credit support (e.g., guarantees), borrowings with third parties, and other ancillary business ventures and real estate operations of the borrower. Our internal ratings range between 1 and 7. An internal rating of 1 reflects the lowest likelihood of loss and a 7 reflects the highest likelihood of loss. The characteristics associated with each risk rating is as follows:
| ● | Risk Rating 1 through 3 – Instruments with minimal to marginally acceptable risk. |
| ● | Risk Rating 4 - Instruments with potential weaknesses identified (Special mention). |
| ● | Risk Rating 5 - Instruments with well-defined weaknesses that may result in possible losses (Substandard). |
| ● | Risk Rating 6 – Instruments that are unlikely to be repaid in full and will probably result in losses (Doubtful). |
| ● | Risk Rating 7 – Instrument that will not be repaid in full and losses will occur (Loss). |
We have a limited history of incurred losses and consequently have elected to employ external data to perform our expected credit loss calculation. We utilize a probability of default (“PD”) and loss given default (“LGD”) methodology. Our model’s historic inputs consider PD and LGD data for residential care facilities published by the Federal Housing Administration along with Standards & Poor’s one-year global corporate default rates. Our historical loss rates revert to historical averages after 36 periods. Our model’s current conditions and supportable forecasts consider internal credit ratings, current and projected U.S. unemployment rates published by the U.S. Bureau of Labor Statistics and the Federal Reserve Bank of St. Louis and the weighted average life to maturity of the underlying financial asset.
Periodically, the Company may identify an individual loan for impairment. A loan is considered impaired when, based on current information and events, it is probable that we will be unable to collect all amounts due as scheduled according to the contractual terms of the loan agreements. Our assessment of collectibility considers several factors, including, among other things, payment history, the financial strength of the borrower and any guarantors, historical operations and operating trends, current and future economic conditions, expectations of performance (which includes known substantial doubt about an operator’s ability to continue as a going concern) and the value of the underlying collateral of the agreement, if any. Consistent with this definition, all loans on non-accrual status may be deemed impaired. To the extent circumstances improve and the risk of collectibility is diminished, we will return these loans to full accrual status. When we identify a loan impairment, the loan is written down to the present value of the expected future cash flows. In cases where expected future cash flows are not readily determinable, the loan is written down to the fair value of the underlying collateral. We may base our valuation on a loan’s observable market price, if any, or the fair value of collateral, net of sales costs, if the repayment of the loan is expected to be provided solely by the sale of the collateral. Financial instruments are charged off against the allowance for credit losses when collectibility is determined to be permanently impaired.
We account for impaired loans using (a) the cost-recovery method, and/or (b) the cash basis method. We generally utilize the cost-recovery method for impaired loans for which impairment reserves were recorded. Under the cost-recovery method, we apply cash received against the outstanding loan balance prior to recording interest income. Under the cash basis method, we apply cash received to principal or interest income based on the terms of the agreement.
Investments in Unconsolidated Joint Ventures
We account for our investments in unconsolidated joint ventures using the equity method of accounting as we exercise significant influence, but do not control the entities.
F-16
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Under the equity method of accounting, the net equity investments of the Company are reflected in the accompanying Consolidated Balance Sheets and the Company’s share of net income and comprehensive income from the joint ventures are included in the accompanying Consolidated Statements of Operations and Consolidated Statements of Comprehensive Income, respectively.
On a periodic basis, management assesses whether there are any indicators that the value of the Company’s investments in the unconsolidated joint ventures may be other-than-temporarily-impaired. An investment is impaired only if management’s estimate of the value of the investment is less than the carrying value of the investment, and such a decline in value is deemed to be other than-temporary. To the extent impairment has occurred, the loss is measured as the excess of the carrying amount of the investment over the estimated fair value of the investment. The estimated fair value of the investment is determined using a discounted cash flow model which is a Level 3 valuation. We consider a number of assumptions that are subject to economic and market uncertainties including, among others, rental rates, operating costs, capitalization rates, holding periods and discount rates.
Cash and Cash Equivalents
Cash and cash equivalents consist of cash on hand and highly liquid investments with a maturity date of three months or less when purchased. These investments are stated at cost, which approximates fair value. The majority of our cash, cash equivalents and restricted cash are held at major commercial banks. Certain cash account balances exceed FDIC insurance limits of $
Restricted Cash
Restricted cash consists primarily of liquidity deposits escrowed for tenant obligations required by us pursuant to certain contractual terms and other deposits required by the U.S. Department of Housing and Urban Development (“HUD”) in connection with our mortgage borrowings guaranteed by HUD.
Deposits
We obtain liquidity deposits and other deposits, security deposits and letters of credit from certain operators pursuant to our lease and mortgage agreements. These generally represent the rental and/or mortgage interest for periods ranging from to
The liquidity deposits and other deposits, security deposits and the letters of credit may be used in the event of lease and/or loan defaults, subject to applicable limitations under bankruptcy law with respect to operators filing under Chapter 11 of the U.S. Bankruptcy Code. Liquidity deposits and other deposits are recorded as restricted cash on our Consolidated Balance Sheets with the offset recorded as a liability in accrued expenses and other liabilities on our Consolidated Balance Sheets. Security deposits related to cash received from the operators are primarily recorded in cash and cash equivalents on our Consolidated Balance Sheets with a corresponding offset in accrued expenses and other liabilities on our Consolidated Balance Sheets. Additional security for rental and mortgage interest revenue from operators is provided by covenants regarding minimum working capital and net worth, liens on accounts receivable and other operating assets of the operators, provisions for cross-default, provisions for cross-collateralization and by corporate or personal guarantees.
F-17
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Goodwill Impairment
We test goodwill for potential impairment at least annually in the fourth quarter, or more frequently if an event or other circumstance indicates that we may not be able to recover the carrying amount of the net assets of the reporting unit. In evaluating goodwill for impairment, we may assess qualitative factors to determine whether it is more likely than not that the fair value of a reporting unit is less than its carrying amount. If we bypass the qualitative assessment, or if we conclude that it is more likely than not that the fair value of a reporting unit is less than its carrying value, then we perform a quantitative impairment test by comparing the fair value of a reporting unit with its carrying amount.
In evaluating goodwill for impairment, we assess qualitative factors such as a significant decline in real estate valuations, current macroeconomic conditions, state of the equity and capital markets and our overall financial and operating performance or a significant decline in the value of our market capitalization, to determine whether it is more likely than not that the fair value of our reporting unit is less than its carrying amount. Goodwill is not deductible for tax purposes. We have had
Income Taxes
Omega and its wholly-owned subsidiaries were organized to qualify for taxation as a REIT under Section 856 through 860 of the Internal Revenue Code (“Code”). As long as we qualify as a REIT; we will not be subject to federal income taxes on the REIT taxable income that we distributed to stockholders, subject to certain exceptions. However, with respect to certain of our subsidiaries that have elected to be treated as taxable REIT subsidiaries (“TRSs”), we record income tax expense or benefit, as those entities are subject to federal income tax similar to regular corporations. Omega OP is a pass-through entity for United States federal income tax purposes.
We account for deferred income taxes using the asset and liability method and recognize deferred tax assets and liabilities for the expected future tax consequences of events that have been included in our financial statements or tax returns. Under this method, we determine deferred tax assets and liabilities based on the differences between the financial reporting and tax bases of assets and liabilities using enacted tax rates in effect for the year in which the differences are expected to reverse. Any increase or decrease in the deferred tax liability that results from a change in circumstances, and that causes us to change our judgment about expected future tax consequences of events, is included in the tax provision when such changes occur. Deferred income taxes also reflect the impact of operating loss and tax credit carry-forwards. A valuation allowance is provided if we believe it is more likely than not that all or some portion of the deferred tax asset will not be realized. Any increase or decrease in the valuation allowance that results from a change in circumstances, and that causes us to change our judgment about the realizability of the related deferred tax asset, is included in the tax provision when such changes occur.
We are subject to certain state and local income tax, franchise taxes and foreign taxes. The expense associated with these taxes are included in income tax expense on the Consolidated Statements of Operations.
Stock-Based Compensation
We recognize stock-based compensation expense adjusted for estimated forfeitures to employees and directors, in general and administrative in our Consolidated Statements of Operations on a straight-line basis over the requisite service period of the awards.
F-18
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Deferred Financing Costs and Original Issuance Premium and/or Discounts for Debt Issuance
External costs incurred from the placement of our debt are capitalized and amortized on a straight-line basis over the terms of the related borrowings which approximates the effective interest method. Deferred financing costs related to our revolving line of credit are included in other assets on our Consolidated Balance Sheets and deferred financing costs related to our other borrowings are included as a direct deduction from the carrying amount of the related liability on our Consolidated Balance Sheets. Original issuance premium or discounts reflect the difference between the face amount of the debt issued and the cash proceeds received and are amortized on a straight-line basis over the term of the related borrowings. All premiums and discounts are recorded as an addition to or reduction from debt on our Consolidated Balance Sheets. Amortization of deferred financing costs and original issuance premiums or discounts totaled $
Earnings Per Share
The computation of basic earnings per share/unit (“EPS”) is computed by dividing net income available to common stockholders by the weighted-average number of shares of common stock outstanding during the relevant period. Diluted EPS is computed using the treasury stock method, which is net income divided by the total weighted-average number of common outstanding shares plus the effect of dilutive common equivalent shares during the respective period. Dilutive common shares reflect the assumed issuance of additional common shares pursuant to certain of our share-based compensation plans, including restricted stock and profit interest units, performance restricted stock and profit interest units, the assumed issuance of additional shares related to Omega OP Units held by outside investors.
Noncontrolling Interests and Redeemable Limited Partnership Unitholder Interests
Noncontrolling interests is the portion of equity not attributable to the respective reporting entity. We present the portion of any equity that we do not own in consolidated entities as noncontrolling interests and classify those interests as a component of total equity, separate from total stockholders’ equity on our Consolidated Balance Sheets. We include net income attributable to the noncontrolling interests in net income in our Consolidated Statements of Operations.
As our ownership of a controlled subsidiary increases or decreases, any difference between the aggregate consideration paid to acquire the noncontrolling interests and our noncontrolling interest balance is recorded as a component of equity in additional paid-in capital, so long as we maintain a controlling ownership interest.
The noncontrolling interest for Omega represents the outstanding Omega OP Units held by outside investors and interests in a consolidated real estate joint venture not fully owned by Omega. Each of the Omega OP Units (other than the Omega OP Units owned by Omega) is redeemable at the election of the Omega OP Unit holder for cash equal to the then-fair market value of one share of Omega common stock, par value $
Foreign Operations
The U.S. dollar (“USD”) is the functional currency for our consolidated subsidiaries operating in the U.S. The functional currency for our consolidated subsidiaries operating in the U.K. is the British Pound (“GBP”). Total revenues from our consolidated U.K. operating subsidiaries were $
F-19
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
For our consolidated subsidiaries whose functional currency is not the USD, we translate their financial statements into the USD. We translate assets and liabilities at the exchange rate in effect as of the financial statement date. Revenue and expense accounts are translated using an average exchange rate for the period. Gains and losses resulting from translation are included in accumulated other comprehensive income (loss) (“AOCI”), as a separate component of equity and a proportionate amount of gain or loss is allocated to noncontrolling interests, if applicable.
We and certain of our consolidated subsidiaries may have intercompany and third-party debt that is not denominated in the entity’s functional currency. When the debt is remeasured against the functional currency of the entity, a gain or loss can result. The resulting adjustment is reflected in results of operations, unless it is intercompany debt that is deemed to be long-term in nature in which case the adjustments are included in AOCI and a proportionate amount of gain or loss is allocated to noncontrolling interests, if applicable.
Derivative Instruments
We are exposed to, among other risks, the impact of changes in foreign currency exchange rates as a result of our investments in the U.K. and interest rate risk related to our capital structure. As a matter of policy, we do not use derivatives for trading or speculative purposes. Our risk management program is designed to manage the exposure and volatility arising from these risks, and utilizes foreign currency forward contracts, interest rate swaps and debt issued in foreign currencies to offset a portion of these risks.
To qualify for hedge accounting, derivative instruments used for risk management purposes must effectively reduce the risk exposure that they are designed to hedge. We formally document all relationships between hedging instruments and hedged items, as well as our risk-management objectives and strategy for undertaking various hedge transactions. This process includes designating all derivatives that are part of a hedging relationship to specific forecasted transactions as well as recognized liabilities or assets on the Consolidated Balance Sheets. In addition, at the inception of a qualifying cash flow hedging relationship, the underlying transaction or transactions, must be, and are expected to remain, probable of occurring in accordance with the Company’s related assertions. The Company recognizes all derivative instruments, including embedded derivatives required to be bifurcated, as assets or liabilities on the Consolidated Balance Sheets at fair value which is determined using a market approach and Level 2 inputs. Changes in the fair value of derivative instruments that are not designated in hedging relationships or that do not meet the criteria of hedge accounting are recognized in earnings. For derivatives designated in qualifying cash flow hedging relationships, the gain or loss on the derivative is recognized in AOCI as a separate component of equity and a proportionate amount of gain or loss is allocated to noncontrolling interest, if applicable.
If it is determined that a derivative instrument ceases to be highly effective as a hedge, or that it is probable the underlying forecasted transaction will not occur, the Company discontinues its cash flow hedge accounting prospectively and records the appropriate adjustment to earnings based on the current fair value of the derivative instrument. For net investment hedge accounting, upon sale or liquidation of our U.K. investment, the cumulative balance of the remeasurement value is reclassified to earnings.
Segments
We conduct our operations and report financial results as
Reclassification
Certain line items on our Consolidated Balance Sheets, Consolidated Statements of Changes in Equity and Consolidated Statements of Cash Flows and have been reclassified to conform to the current period presentation.
F-20
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Recently Adopted Accounting Pronouncements
ASU – 2021-05, Leases (Topic 842): Lessors – Certain Leases with Variable Lease Payments
On July 19, 2021, the Financial Accounting Standards Board (“FASB”) issued Accounting Standards Update (“ASU”) 2021-05. This guidance requires lessors to classify leases with variable lease payments, that do not depend on an index or rate, as an operating lease on the commencement date of the lease if specified criteria are met. The guidance is effective for fiscal years beginning after December 15, 2021, including interim periods within those fiscal years. Early adoption is permitted. We early adopted this guidance prospectively effective July 1, 2021. The adoption of the guidance did not have an impact on our consolidated financial statements.
ASU – 2020-04, Financial Instruments – Reference Rate Reform (Topic 848)
On March 12, 2020, the FASB issued ASU 2020-04, which contains optional practical expedients for a limited period of time to ease the potential burden in accounting for (or recognizing the effects of) reference rate reform on financial reporting for contracts, hedging relationships, and other transactions that reference the London Interbank Offered Rate (“LIBOR”). The guidance may be elected over time until December 31, 2022, as reference rate reform activities occur. The Company has several derivative instruments (See Note 15 – Derivatives and Hedging), a $
ASU – 2016-13, Financial Instruments - Credit Losses (Topic 326)
In June 2016, the FASB issued ASU 2016-13, which changed the impairment model for most financial assets. The new model uses a forward-looking expected loss method, which will generally result in earlier recognition of allowances for credit losses. The new approach requires the calculation of expected lifetime credit losses and is applied to financial assets measured at amortized cost, including loans, as well as certain off-balance sheet credit exposures such as unfunded loan commitments. The allowance for credit loss on the loans is a valuation amount that is deducted from the amortized cost basis of the loans not held at fair value to present the net amount expected to be collected over the contractual term of the loans.
ASU 2016-13 specifically excludes from its scope receivables arising from operating leases accounted for under Topic 842. We adopted ASU 2016-13 on January 1, 2020 using the modified retrospective approach and we recorded an initial $
Pre-adoption balance as of |
Impact of adopting |
Post-adoption balance as of |
||||
Financial Statement Line Item |
December 31, 2019 |
Topic 326 |
January 1, 2020 |
|||
(in thousands) |
||||||
Mortgage notes receivable - net |
$ |
|
$ |
( |
$ |
|
Investment in direct financing leases - net |
|
( |
|
|||
Other investments - net |
|
( |
|
|||
Off-balance sheet commitments |
|
( |
|
|||
Total |
$ |
|
$ |
( |
$ |
|
F-21
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
ASU – 2016-02, Leases (Topic 842)
On January 1, 2019, we adopted ASC 842, Leases (“Topic 842”) using the modified retrospective method. Topic 842 sets out the principles for the recognition, measurement, presentation and disclosure of leases for both parties to a contract (i.e., lessees and lessors). At the inception of a lease and over its term, we evaluate each lease to determine the proper lease classification. Certain of these leases provide our operators or us the contractual right to use and economically benefit from all of the physical space specified in the lease, therefore we have determined that they should be evaluated as lease arrangements.
Upon adoption of Topic 842, we applied the package of practical expedients that allowed us to not reassess (i) whether any expired or existing contracts are or contain leases, (ii) lease classification for any expired or existing leases and (iii) initial direct costs for any expired or existing leases. Furthermore, we applied the optional transition method, which allowed us to initially apply Topic 842 at the adoption date and recognize a cumulative effect adjustment to the opening balance of equity in the period of adoption. During the year ended December 31, 2019, we made an adjustment of approximately $
NOTE 3 – REAL ESTATE ACQUISITIONS
2021 Acquisitions and Other
The following table summarizes the significant asset acquisitions that occurred in 2021:
Number of |
Total Real Estate |
Initial |
||||||||||
|
Facilities |
|
|
Assets Acquired(1) |
|
Annual |
||||||
Period |
SNF |
ALF |
Specialty |
Country/State |
(in millions) |
Cash Yield(2) |
||||||
Q1 |
|
— |
|
|
|
AZ, CA, FL, IL, NJ, OR, PA, TN, TX, VA, WA |
$ |
|
|
% |
||
Q1 |
|
— |
— |
FL |
|
|
% |
|||||
Q3 |
— |
|
— |
U.K. |
|
|
% |
|||||
Total |
|
|
|
|
|
|
$ |
|
|
|||
| (1) |
Excludes $ |
| (2) | Initial annual cash yield reflects the initial annual contractual cash rent divided by the purchase price. |
On January 20, 2021, we acquired
Construction in progress investments
During the third quarter of 2021, we purchased a real estate property located in Washington, D.C. (not reflected in the table above) for approximately $
F-22
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
2020 Acquisitions
The following table summarizes the significant asset acquisitions that occurred in 2020:
Number of |
Total Real Estate |
Initial |
|||||||||
|
Facilities |
|
|
Assets Acquired |
|
Annual |
|||||
Period |
SNF |
ALF |
Country/State |
(in millions) |
Cash Yield(1) |
||||||
Q1 |
|
— |
|
|
U.K. |
$ |
|
|
% |
||
Q1 |
|
— |
IN |
|
|
% |
|||||
Q2 |
|
— |
OH |
|
|
% |
|||||
Q4 |
|
|
VA |
|
|
% |
|||||
Total |
|
|
|
|
|
$ |
|
|
|||
| (1) | Initial annual cash yield reflects the initial annual contractual cash rent divided by the purchase price. |
2019 Acquisitions and Other
The following table summarizes the significant transactions that occurred in 2019:
Number of |
Total Real Estate |
Initial |
||||||||||||
|
Facilities |
|
|
Assets Acquired |
|
|
Annual |
|||||||
Period |
SNF |
ALF |
Specialty |
MOB |
Country/State |
(in millions) |
Cash Yield(1) |
|||||||
Q1 |
|
|
— |
— |
— |
|
OH |
$ |
|
(3) |
|
|
% |
|
Q2 |
|
|
|
|
|
|
CA, CT, IN, NV, SC, TN, TX |
|
|
(2) |
|
|
% |
|
Q2 |
|
|
|
|
— |
|
PA, VA |
|
|
(3) |
|
|
% |
|
Q3 |
|
— |
— |
— |
|
NC, VA |
|
|
|
|
% |
|||
Q4 |
|
|
— |
— |
|
FL, ID, KY, LA, MS, MO, MT, NC |
|
|
|
|
% |
|||
Total |
|
|
|
|
|
|
|
$ |
|
|
|
|||
| (1) | Initial annual cash yield reflects the initial annual contractual cash rent divided by the purchase price. |
| (2) | The acquisition was accounted for as a business combination. The other 2019 acquisitions were accounted for as asset acquisitions. |
| (3) | Acquired via a deed-in-lieu of foreclosure. |
Encore Portfolio Acquisition
On October 31, 2019, we completed the $
The following table highlights the fair value of the assets acquired and liabilities assumed on October 31, 2019:
(in thousands) |
|||
Fair value of net assets acquired: |
|||
Real estate assets |
$ |
|
|
Other investments |
|
|
|
Contractual receivables |
|
||
Cash |
|
|
|
Other assets |
|
|
|
Total investments |
|
||
Secured borrowings |
( |
||
Accrued expenses and other liabilities |
( |
||
Fair value of net assets acquired |
$ |
|
|
F-23
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
MedEquities Merger
On May 17, 2019, we completed our acquisition by merger of MedEquities (the “MedEquities Merger”) and its subsidiary operating partnership and the general partner of its subsidiary operating partnership.
In connection with the MedEquities Merger, we issued approximately
Our purchase price allocation was finalized during the second quarter of 2020, with no material adjustments recorded. The following table highlights the final fair value of the assets acquired and liabilities assumed on May 17, 2019:
(in thousands) |
|||
Fair value of net assets acquired: |
|||
Real estate assets |
$ |
|
|
Mortgage notes receivable |
|
|
|
Other investments |
|
|
|
Investment in unconsolidated joint venture |
|
|
|
Cash |
|
|
|
Contractual receivables |
|
|
|
Other assets (1) |
|
|
|
Total investments |
|
||
Debt (2) |
( |
||
Accrued expenses and other liabilities (3) |
( |
||
Fair value of net assets acquired |
$ |
|
|
| (1) |
Includes approximately $ |
| (2) |
In connection with the MedEquities Merger on May 17, 2019, we assumed a $ |
| (3) |
Includes approximately $ |
The MedEquities facilities acquired in 2019 are included in our results of operations from the date of acquisition. For the period from May 17, 2019 through December 31, 2019, we recognized approximately $
Pro Forma Acquisition Results
The following unaudited pro forma information presents consolidated financial information as if the MedEquities Merger occurred on January 1, 2019. In the opinion of management, all significant necessary adjustments to reflect the effect of the merger have been made. The following pro forma information is not indicative of future operations.
F-24
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Pro Forma |
|||
Year Ended December 31, 2019 |
|||
(in thousands, except per share amounts, unaudited) |
|||
|
|||
Pro forma revenues |
$ |
|
|
Pro forma net income |
$ |
|
|
Earnings per share – diluted: |
|||
Net income – as reported |
$ |
|
|
Net income – pro forma |
$ |
|
|
NOTE 4 – ASSETS HELD FOR SALE, DISPOSITIONS AND IMPAIRMENTS
Periodically, we will sell facilities to reduce our concentration in certain operators, geographies, and non-strategic assets or due to the exercise of a tenant purchase option.
In December 2021, we entered into an agreement to sell
As of February 7, 2022, the remaining
The following is a summary of our assets held for sale:
December 31, |
December 31, |
||||
2021 |
|
2020 |
|||
Number of facilities held for sale |
|||||
Amount of assets held for sale (in thousands) |
$ |
|
$ |
|
|
Asset Sales
During the year ended December 31, 2021, we sold
During the year ended December 31, 2020, we sold
During the year ended December 31, 2019, we sold
Real Estate Impairments
During the year ended December 31, 2021, we recorded impairments of approximately $
F-25
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
During the year ended December 31, 2020, we recorded impairments of approximately $
During the year ended December 31, 2019, we recorded impairments of approximately $
To estimate the fair value of the facilities determined to be held for sale, for the impairments noted above, we utilized a market approach which considered binding sale agreements (a Level 1 input) or non-binding offers from unrelated third parties and/or broker quotes (a Level 3 input).
NOTE 5 – CONTRACTUAL RECEIVABLES AND OTHER RECEIVABLES AND LEASE INDUCEMENTS
Contractual receivables relate to the amounts currently owed to us under the terms of our lease and loan agreements. Effective yield interest receivables relate to the difference between the interest income recognized on an effective yield basis over the term of the loan agreement and the interest currently due to us according to the contractual agreement. Straight-line rent receivables relate to the difference between the rental revenue recognized on a straight-line basis and the amounts currently due to us according to the contractual agreement. Lease inducements result from value provided by us to the lessee, at the inception, modification or renewal of the lease, and are amortized as a reduction of rental income over the non-cancellable lease term.
A summary of our net receivables by type is as follows:
|
December 31, |
December 31, |
|||||
|
2021 |
|
2020 |
|
|||
(in thousands) |
|||||||
Contractual receivables – net |
$ |
|
$ |
|
|||
Effective yield interest receivables |
$ |
|
$ |
|
|||
Straight-line rent receivables |
|
|
|
|
|||
Lease inducements |
|
|
|
|
|||
Other receivables and lease inducements |
$ |
|
$ |
|
|||
Agemo Holdings, LLC
From August 2021 through October 2021 and in December 2021, Agemo Holdings, LLC (“Agemo”), failed to pay contractual rent and interest due under their lease and loan agreements, but paid rent and interest in November 2021. Agemo was formed in May 2018 by Signature Healthcare, LLC, as part of an out-of-court restructuring agreement, to be the holding company of their leases and loans with Omega.
F-26
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
We placed Agemo on a cash basis of revenue recognition during the third quarter of 2020 as collection of substantially all contractual lease payments due from them was deemed no longer probable because of information received regarding substantial doubt of their ability to continue as a going concern. As a result, we wrote-off approximately $
As part of the 2018 restructuring agreement with Agemo discussed above, Omega agreed to, among other terms, defer rent of $
Guardian Healthcare
From October 2021 through December 2021, Guardian Healthcare (“Guardian”) failed to make contractual rent and interest payments under its lease agreement for
As a result of Guardian’s non-payment of contractual rent and the anticipated restructuring noted above, in the fourth quarter of 2021, we placed Guardian on a cash basis of revenue recognition and wrote-off approximately $
Gulf Coast
During the second quarter of 2021, Gulf Coast stopped paying contractual rent under its master lease agreement because of on-going liquidity issues. Gulf Coast operates
F-27
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
As a result of Gulf Coast’s default under its master lease agreement, in August 2021, we exercised our right to accelerate the full amount of rent due under Gulf Coast’s master lease agreement. On October 14, 2021, Gulf Coast commenced voluntary cases under Chapter 11 of the U.S. Bankruptcy Code in the U.S. Bankruptcy Court for the District of Delaware (the “Bankruptcy Court”). The payment of our accelerated rent will be subject to the Bankruptcy Code and approval of the bankruptcy court in Gulf Coast’s Chapter 11 cases. As described in Gulf Coast’s filings with the Bankruptcy Court, we have entered into a Restructuring Support Agreement (the “Support Agreement”) that forms the basis for Gulf Coast’s intended restructuring and liquidation. The Support Agreement establishes a timeline for the implementation of Gulf Coast’s planned restructuring and liquidation, including the transition of management of the operations of the facilities to a third-party operator. As part of the Support Agreement, we committed to provide up to $
As a result of Gulf Coast’s non-payment of contractual rent, in the second quarter of 2021, we placed Gulf Coast on a cash basis of revenue recognition and wrote-off straight-line rent receivable balances of $
In August 2021, following an assertion by the holders of the Subordinated Debt that our prior exercise of offset rights had resulted in defaults under the terms of the Subordinated Debt, we also filed suit in the Circuit Court for Baltimore County against the holders of the Subordinated Debt seeking a declaratory judgment to, among other items, declare that the aggregate amount of unpaid rent due from Gulf Coast under the master lease agreement exceeds all amounts which otherwise would be due and owing by Omega Obligor under the Subordinated Debt, and that all principal and interest due and owing under the Subordinated Debt may be (and was) offset in full as of December 31, 2021. In October 2021, the defendants in the case filed a motion to dismiss for lack of personal jurisdiction. While Omega believes that Omega Obligor is entitled to the enforcement of the offset rights sought in the action, the outcome of litigation is unpredictable, and Omega cannot predict the outcome of the declaratory judgment action.
Daybreak
During the third quarter of 2017, we placed Daybreak on a cash basis for revenue recognition as a result of nonpayment of funds owed to us. During the fourth quarter of 2017, we executed a Settlement and Forbearance Agreement with Daybreak which permitted Daybreak to defer payments up to
F-28
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
On January 30, 2019, we entered into a Second Amendment to the Settlement and Forbearance Agreement under which we agreed to defer approximately $
During 2020, as part of our plan to transition and sell our Daybreak facilities, we transitioned
Other straight-line receivables and write-offs
In addition to the Guardian and Gulf Coast straight-line receivable write-offs in 2021 discussed above, we wrote-off straight-line rent receivable balances of $
In addition to the write-off of Agemo’s contractual receivables, straight-line rent receivables, and lease inducements in the third quarter of 2020 discussed above, we wrote-off approximately $
During 2019, we wrote-off approximately $
Lease Inducements
For the years ended December 31, 2021, 2020 and 2019, we provided fundings of $
F-29
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
NOTE 6 –LEASES
Lease Income
The following table summarizes the Company’s rental income from operating leases:
Year Ended December 31, |
|||||||||
2021 |
2020 |
2019 |
|||||||
(in thousands) |
|||||||||
Rental income – operating leases |
$ |
|
$ |
|
$ |
|
|||
Variable lease income – operating leases |
|
|
|
||||||
Total rental income |
$ |
|
$ |
|
$ |
|
|||
Our variable lease income primarily represents the reimbursement of real estate taxes and ground lease expenses by operators that Omega pays directly.
The following amounts reflect the future minimum lease payments due to us for the remainder of the initial terms of our operating leases as of December 31, 2021:
(in thousands) |
|||
2022 |
$ |
|
|
2023 |
|
||
2024 |
|
||
2025 |
|
||
2026 |
|
||
Thereafter |
|
||
Total |
$ |
|
|
Lease Costs
As of December 31, 2021, the Company is a lessee under ground leases and/or facility leases related to
The following table summarizes the balance sheet information related to leases where the Company is a lessee:
December 31, |
December 31, |
December 31, |
|||||||
2021 |
2020 |
2019 |
|||||||
(in thousands) |
|||||||||
$ |
|
$ |
|
$ |
|
||||
$ |
|
$ |
|
$ |
|
||||
F-30
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Direct Financing Leases
The components of investments in direct financing leases consist of the following:
|
December 31, |
December 31, |
|||||
|
2021 |
|
2020 |
|
|||
(in thousands) |
|||||||
Minimum lease payments receivable |
$ |
|
$ |
|
|||
Less unearned income |
|
( |
|
( |
|||
Investment in direct financing leases |
|
|
|
|
|||
Less allowance for credit losses on direct financing leases |
|
( |
|
( |
|||
Investment in direct financing leases – net |
$ |
|
$ |
|
|||
Properties subject to direct financing leases |
|
|
|
|
|||
Number of direct financing leases |
|
|
|
|
|||
Orianna Direct Financing Lease
On January 11, 2019, pursuant to a bankruptcy court order, affiliates of Orianna Health Systems (“Orianna”) purchased the remaining
On January 16, 2019, the bankruptcy court confirmed Orianna’s plan of reorganization, creating a Distribution Trust (the “Trust”) to distribute the proceeds from Orianna’s sale of the remaining
In March 2019, we received updated information from the Trust indicating diminished collectibility of the accounts receivable owed to us. As a result, we recorded an additional $
NOTE 7 - MORTGAGE NOTES RECEIVABLE
As of December 31, 2021, mortgage notes receivable relate to
F-31
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
The principal amounts outstanding of mortgage notes receivable, net of allowances, were as follows:
December 31, |
December 31, |
||||||
|
2021 |
|
2020 |
|
|||
(in thousands) |
|||||||
Mortgage note due |
$ |
|
$ |
|
|||
Mortgage notes due |
|
|
|
|
|||
Other mortgage notes outstanding(2) |
|
|
|
|
|||
Mortgage notes receivable, gross |
|
|
|
|
|||
Allowance for credit losses on mortgage notes receivable |
|
( |
|
( |
|||
Total mortgage notes receivable — net |
$ |
|
$ |
|
|||
| (1) |
Approximates the weighted average interest rate on |
| (2) |
Other mortgage notes outstanding have a weighted average interest rate of |
Mortgage Note due
On January 17, 2014, we entered into a $
As discussed in Note 9 – Allowance for Credit Losses, we reduced the risk rating on the mortgage loan from a 4 to a 5 during the third quarter of 2021, primarily due to the increased likelihood of a restructuring that would result in the modification of the mortgage loan terms. The reduction in risk rating increased our reserve on the mortgage loan, determined using our PD and LGD credit loss model, to $
F-32
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Mortgage Notes due
At December 31, 2021, the $
| ● |
$ |
| ● |
Additional borrowings in the form of incremental facility mortgages, construction and/or improvement mortgages with maturities through |
| ● |
$ |
| ● |
$ |
| ● |
$ |
The mortgage notes with Ciena are cross-defaulted and cross-collateralized with our existing master lease and other investment notes with the operator.
F-33
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Other mortgage notes outstanding
Mortgage Note due
On July 1, 2021, we financed
Mortgage Note due
In connection with the MedEquities Merger on May 17, 2019, the Company acquired a first mortgage lien issued to Lakeway Realty, L.L.C, an unconsolidated joint venture discussed in Note 11 – Investments in Joint Ventures, in the original principal amount of approximately $
NOTE 8 - OTHER INVESTMENTS
Our other investments consist of fixed and variable rate loans to our operators and/or their principals to fund working capital and capital expenditures. These loans may be either unsecured or secured by the collateral of the borrower. Interest revenue on these loans is included within other investment income on the Consolidated Statement of Operations. As of December 31, 2021, we had
|
December 31, |
December 31, |
|||||
|
2021 |
|
2020 |
||||
(in thousands) |
|||||||
Other investment notes due |
$ |
|
|
$ |
|
||
Other investment notes due |
|
|
|
||||
Other investment note due |
|
|
|
||||
Other investment notes due |
|
|
|
|
|||
Other investment notes outstanding (2) |
|
|
|
|
|||
Total other investments, gross |
|
|
|||||
Allowance for credit losses on other investments |
( |
( |
|||||
Total other investments - net |
$ |
|
$ |
|
|||
| (1) | Approximate weighted average interest rate as of December 31, 2021. |
| (2) |
Other investment notes have a weighted average interest rate of |
F-34
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Other investment notes due 2024
Our other investment notes due in 2024 consists of two secured term loans with Genesis with initial borrowings of $
Other investment notes due 2024-2025
Our other investment notes due in 2024-2025 consist of a $
As discussed in Note 5 – Contractual Receivables and Other Receivables and Lease Inducements, Agemo failed to pay contractual rent and interest to us from August 2021 through October 2021 and in December 2021. We have continued to monitor the fair value of the collateral associated with these loans on a quarterly basis. In the third quarter of 2021, we recorded an additional provision for credit loss of $
We previously had two other loans with Agemo affiliates that were repaid during 2020: $
At December 31, 2021, the total carrying value of our loans outstanding with Agemo and its affiliates, net of allowances for credit losses, is approximately $
F-35
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Other investment note due 2023
Our other investment note due in 2023 consists of a $
Other investment notes due 2030
In 2015 and 2017, we entered into two separate $
As a result of entering into the $
Other investment notes outstanding
As of December 31, 2021, our other investment notes outstanding represents
Gulf Coast – DIP Facility
As discussed in Note 5 – Contractual Receivables and Other Receivables and Lease Inducements, in October 2021, we provided an up to $
F-36
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Given the uncertainty and complexity surrounding the bankruptcy process and the deteriorated credit of Gulf Coast, we evaluated the DIP facility on an individual basis and elected to measure the risk of loss on the DIP Facility based on the fair value of the collateral. Based on the cash forecasts provided by Gulf Coast as part of the Support Agreement and on-going monthly reporting, we estimate that the collateral will have insufficient value to support the loan at maturity and that we will be unable to collect on substantially all principal amounts advanced to Gulf Coast under the DIP Facility. Upon funding, we fully reserved all principal amounts advanced under the DIP Facility. In the fourth quarter of 2021, we recorded reserves of $
Working Capital Loan - $
As discussed in Note 5 – Contractual Receivables and Other Receivables and Lease Inducements, in November 2021, we entered into a $
Revolving Credit Facility - $
On October 1, 2021, the Company amended the terms of a $
As discussed in Note 23 – Subsequent Events, in January and February 2022, this operator paid contractual interest under the credit facility but failed to pay contractual rent due under its lease agreement. The operator has asked for a short-term rent deferral, and negotiations are on-going.
Second Spring Healthcare Investments
On April 17, 2020, we provided a $
Sellers Note - $30 million
In connection with transitioning facilities associated with Orianna Health Systems, a former operator, in January 2019 we issued a $
F-37
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
NOTE 9 – ALLOWANCE FOR CREDIT LOSSES
A rollforward of our allowance for credit losses, summarized by financial instrument type and internal credit risk rating, for the years ended December 31, 2021 and 2020 is as follows:
Rating |
Financial Statement Line Item |
Allowance for Credit Loss as of December 31, 2020 |
Provision (recovery) for Credit Loss for the year ended December 31, 2021 |
Write-offs charged against allowance for the year ended December 30, 2021 |
Allowance for Credit Loss as of December 31, 2021 |
|||||
(in thousands) |
||||||||||
2 |
Mortgage notes receivable |
$ |
|
$ |
( |
$ |
— |
$ |
|
|
3 |
Mortgage notes receivable |
|
|
— |
|
|||||
4 |
Mortgage notes receivable |
|
( |
(1) |
— |
|
||||
5 |
Mortgage notes receivable |
|
( |
— |
|
|||||
6 |
Mortgage notes receivable |
|
|
(1) |
— |
|
||||
Sub-total |
|
|
— |
|
||||||
3 |
Investment in direct financing leases |
|
( |
— |
|
|||||
Sub-total |
|
( |
— |
|
||||||
2 |
Other investments |
|
( |
— |
|
|||||
3 |
Other investments |
|
( |
— |
|
|||||
4 |
Other investments |
|
( |
(2) |
— |
|
||||
5 |
Other investments |
|
|
(3) |
( |
|
||||
6 |
Other investments |
— |
|
(4) |
— |
|
||||
Sub-total |
|
|
( |
|
||||||
2 |
Off-balance sheet note commitments |
|
( |
— |
|
|||||
3 |
Off-balance sheet note commitments |
|
( |
— |
|
|||||
4 |
Off-balance sheet note commitments |
— |
|
— |
|
|||||
4 |
Off-balance sheet mortgage commitments |
|
|
— |
|
|||||
6 |
Off-balance sheet mortgage commitments |
— |
|
— |
|
|||||
Sub-total |
|
( |
— |
|
||||||
Total |
$ |
|
$ |
|
$ |
( |
$ |
|
||
| (1) |
Amount reflects the movement of reserves associated with a $ |
| (2) |
Amount reflects the movement of $ |
| (3) |
The provision includes an additional $ |
| (4) |
Amount reflects the movement of $ |
F-38
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Rating |
Financial Statement Line Item |
Allowance for Credit Loss at December 31, 2019 |
Allowance for Credit Loss on January 1, 2020 |
Provision (recovery) for Credit Loss for the year ended December 31, 2020 |
Write-offs charged against allowance for the year ended December 30, 2020 |
Allowance for Credit Loss as of December 31, 2020 |
||||||
(in thousands) |
||||||||||||
2 |
Mortgage notes receivable |
$ |
— |
$ |
— |
$ |
|
$ |
— |
$ |
|
|
3 |
Mortgage notes receivable |
— |
|
|
— |
|
||||||
4 |
Mortgage notes receivable |
— |
|
|
— |
|
||||||
5 |
Mortgage notes receivable |
— |
|
( |
— |
|
||||||
6 |
Mortgage notes receivable |
|
|
( |
— |
|
||||||
Sub-total |
|
|
|
— |
|
|||||||
3 |
Investment in direct financing leases |
|
|
|
( |
|
||||||
Sub-total |
|
|
|
( |
|
|||||||
2 |
Other investments |
— |
|
( |
— |
|
||||||
3 |
Other investments |
— |
|
|
— |
|
||||||
4 |
Other investments |
— |
|
|
— |
|
||||||
5 |
Other investments |
— |
|
( |
— |
|
||||||
Sub-total |
— |
|
|
— |
|
|||||||
2 |
Off-balance sheet note commitments |
— |
— |
|
— |
|
||||||
3 |
Off-balance sheet note commitments |
— |
— |
|
— |
|
||||||
4 |
Off-balance sheet mortgage commitments |
— |
|
( |
— |
|
||||||
Sub-total |
— |
|
|
— |
|
|||||||
Total |
$ |
|
$ |
|
$ |
|
$ |
( |
$ |
|
||
Included below is a summary of the amortized cost basis of our financial instruments, subject to the allowance for credit losses, by year of origination and our internal risk rating:
Rating |
Financial Statement Line Item |
2021 |
2020 |
2019 |
2018 |
2017 |
2016 |
2015 & older |
Revolving Loans |
Balance as of December 31, 2021 |
||||||||||
(in thousands) |
||||||||||||||||||||
1 |
Mortgage notes receivable |
$ |
— |
$ |
— |
$ |
— |
$ |
— |
$ |
— |
$ |
— |
$ |
|
$ |
— |
$ |
|
|
2 |
Mortgage notes receivable |
— |
|
— |
— |
— |
— |
— |
— |
|
||||||||||
3 |
Mortgage notes receivable |
|
— |
— |
— |
— |
— |
— |
— |
|
||||||||||
4 |
Mortgage notes receivable |
|
|
|
|
|
|
|
— |
|
||||||||||
5 |
Mortgage notes receivable |
— |
— |
— |
— |
— |
— |
|
— |
|
||||||||||
6 |
Mortgage notes receivable |
— |
— |
— |
— |
— |
— |
|
— |
|
||||||||||
Sub-total |
|
|
|
|
|
|
|
— |
|
|||||||||||
3 |
Investment in direct financing leases |
— |
— |
— |
— |
— |
— |
|
— |
|
||||||||||
Sub-total |
— |
— |
— |
— |
— |
— |
|
— |
|
|||||||||||
2 |
Other investments |
— |
— |
— |
— |
— |
— |
— |
|
|
||||||||||
3 |
Other investments |
— |
— |
|
|
— |
— |
|
|
|
||||||||||
4 |
Other investments |
|
— |
|
|
— |
|
— |
— |
|
||||||||||
5 |
Other investments |
— |
— |
— |
|
— |
— |
— |
— |
|
||||||||||
6 |
Other investments |
|
— |
— |
|
— |
|
— |
— |
|
||||||||||
Sub-total |
|
— |
|
|
— |
|
|
|
|
|||||||||||
Total |
$ |
|
$ |
|
$ |
|
$ |
|
$ |
|
$ |
|
$ |
|
$ |
|
$ |
|
||
F-39
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Interest Receivable on Mortgage and Other Investment Loans
We have elected the practical expedient to exclude interest receivable from our allowance for credit losses. As of December 31, 2021 and 2020, $
During the year ended December 31, 2021, we recognized $
NOTE 10 – VARIABLE INTEREST ENTITIES
We hold variable interests in several VIEs through our investing and financing activities. As of December 31, 2021, we have not consolidated any VIEs, as we have concluded that we are not the primary beneficiary of these entities as we either we do not have the power to direct activities that most significantly impact the VIE’s economic performance and/or the variable interest we hold does not obligate us to absorb losses or provide us with the right to receive benefits from the VIE which could potentially be significant.
Below is a summary of our assets, liabilities, collateral and maximum exposure to loss associated with these unconsolidated VIEs as of December 31, 2021 and 2020:
December 31, |
December 31, |
||||||
2021 |
2020 |
||||||
(in thousands) |
|||||||
Assets |
|||||||
Real estate assets – net |
$ |
|
$ |
|
|||
Assets held for sale |
|
— |
|||||
Other investments – net |
|
|
|
||||
Contractual receivables – net |
|
|
|
||||
Straight-line rent receivables |
|
( |
( |
||||
Lease inducement |
|
|
|||||
Total assets |
|
|
|
|
|||
Liabilities |
|||||||
Net in-place lease liability |
( |
( |
|||||
Security deposit |
( |
— |
|||||
Contingent liability |
( |
( |
|||||
Total liabilities |
|
( |
|
( |
|||
Collateral |
|
|
|
|
|||
Letters of credit |
|
— |
( |
||||
Personal guarantee |
|
( |
( |
||||
Other collateral(1) |
|
( |
( |
||||
Total collateral |
|
( |
( |
||||
Maximum exposure to loss |
$ |
|
$ |
|
|||
| (1) |
Amount excludes accounts receivable amounts that Omega has a security interest in as collateral under the two working capital loans with operators that are VIEs. The fair value of the accounts receivable available to Omega was $ |
F-40
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
In determining our maximum exposure to loss from these VIEs, we considered the underlying carrying value of the real estate subject to leases with these operators and other collateral, if any, supporting our other investments, which may include accounts receivable, security deposits, letters of credit or personal guarantees, if any, as well as other liabilities recognized with respect to these operators.
The table below reflects our total revenues from the operators that are considered VIEs for the years ended December 31, 2021, 2020 and 2019:
Year Ended December 31, |
|||||||||||
2021 |
2020 |
2019 |
|||||||||
(in thousands) |
|||||||||||
Revenue |
|
|
|
|
|||||||
Rental income (1) |
$ |
|
$ |
|
$ |
|
|||||
Other investment income |
|
|
|
|
|
|
|||||
Total |
$ |
|
$ |
|
$ |
|
|||||
| (1) |
The rental income for the year ended December 31, 2020, reflects the write-off of approximately $ |
NOTE 11 – INVESTMENTS IN JOINT VENTURES
Unconsolidated Joint Ventures
Omega owns an interest in a number of joint ventures that are accounted for under the equity method. These entities and their subsidiaries are not consolidated by the Company because it does not control, through voting rights or other means, the joint venture. The following is a summary of our investments in unconsolidated joint ventures (dollars in thousands):
Carrying Amount |
|||||||||||||||||
Ownership |
Initial Investment |
Facility |
Facilities at |
December 31, |
December 31, |
||||||||||||
Entity |
% |
Date |
Investment(1) |
Type |
12/31/2021 |
2021 |
|
2020 |
|||||||||
Second Spring Healthcare Investments(2) |
$ |
|
SNF |
— |
$ |
|
|
$ |
|
||||||||
Second Spring II LLC(3) |
|
SNF |
— |
|
|
— |
|||||||||||
Lakeway Realty, L.L.C.(4) |
|
Specialty facility |
|
|
|||||||||||||
Cindat Joint Venture(5) |
|
ALF |
|
|
|||||||||||||
OMG Senior Housing, LLC |
— |
Specialty facility |
|
— |
|
— |
|||||||||||
OH CHS SNP, Inc. |
|
N/A |
N/A |
|
|
||||||||||||
$ |
|
$ |
|
$ |
|
||||||||||||
| (1) | Our investment includes our transaction costs, if any. |
| (2) |
The Company made a loan of $ |
| (3) |
We acquired a |
| (4) |
We acquired an interest in a joint venture that owns the Lakeway Regional Medical Center (the “Lakeway Hospital”) in Lakeway, Texas. Our initial basis difference of approximately $ |
| (5) |
We acquired a |
F-41
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
The following table reflects our income (loss) from unconsolidated joint ventures for the years ended December 31, 2021, 2020 and 2019:
Year Ended December 31, |
|||||||||
Entity |
2021 |
|
2020 |
|
2019 |
||||
(in thousands) |
|||||||||
Second Spring Healthcare Investments(1) |
$ |
|
$ |
|
$ |
|
|||
Second Spring II LLC |
( |
|
|
||||||
Lakeway Realty, L.L.C. |
|
|
|
|
|
||||
Cindat Joint Venture |
|
|
|
|
|
( |
|||
OMG Senior Housing, LLC |
|
( |
|
( |
|
|
|||
OH CHS SNP, Inc. |
|
( |
|
( |
|
|
|||
Total |
$ |
|
$ |
|
$ |
|
|||
| (1) |
The income from this unconsolidated joint venture for the year ended December 31, 2021 includes a $ |
Asset Management Fees
We receive asset management fees from certain joint ventures for services provided. For the years ended December 31, 2021, 2020 and 2019, we recognized approximately $
Other Equity Investments
In the third quarter of 2021, we made an investment of $
NOTE 12 – GOODWILL AND OTHER INTANGIBLES
The following is a summary of our goodwill:
|
(in thousands) |
||
Balance as of December 31, 2020 |
$ |
|
|
Foreign currency translation |
|
( |
|
Balance as of December 31, 2021 |
$ |
|
|
F-42
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
The following is a summary of our lease intangibles as of December 31, 2021 and 2020:
|
December 31, |
December 31, |
|||||
|
2021 |
|
2020 |
||||
(in thousands) |
|||||||
Assets: |
|
|
|
||||
Above market leases |
$ |
|
$ |
|
|||
Accumulated amortization |
|
( |
|
|
( |
||
Net above market leases |
$ |
|
$ |
|
|||
Liabilities: |
|
|
|
||||
Below market leases |
$ |
|
$ |
|
|||
Accumulated amortization |
|
( |
|
|
( |
||
Net below market leases |
$ |
|
$ |
|
|||
For the years ended December 31, 2021, 2020 and 2019, our net amortization related to intangibles was $
NOTE 13 - CONCENTRATION OF RISK
As of December 31, 2021, our portfolio of real estate investments (including properties associated with mortgages, direct financing leases, and assets held for sale) consisted of
At December 31, 2021, we had investments with
At December 31, 2020, we had investments with
At December 31, 2021, the three states in which we had our highest concentration of investments were Florida (
F-43
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
NOTE 14 - BORROWING ARRANGEMENTS
The following is a summary of our long-term borrowings:
|
|
Annual |
|
||||||||
Interest Rate |
|||||||||||
as of |
|||||||||||
December 31, |
December 31, |
December 31, |
|||||||||
|
Maturity |
|
2021 |
|
2021 |
|
2020 |
||||
|
|
|
(in thousands) |
||||||||
Secured borrowings |
|
|
|
|
|
|
|
|
|||
HUD mortgages(1)(2) |
|
% |
$ |
|
$ |
|
|||||
Term loan(3) |
|
|
|
% |
|
|
|||||
Total secured borrowings |
|
|
|||||||||
Unsecured borrowings |
|
|
|
|
|
|
|
|
|||
Revolving borrowings: |
|
||||||||||
2017 Revolving credit facility(4) |
|
|
N/A |
|
— |
|
|
||||
Revolving credit facility(4) |
|
|
|
% |
|
— |
|
— |
|||
Total revolving borrowings |
— |
|
|||||||||
Senior notes and other unsecured borrowings: |
|||||||||||
2023 notes(4)(5) |
|
|
|
% |
|
|
|
|
|||
2024 notes(4) |
|
|
|
% |
|
|
|
|
|||
2025 notes(4) |
|
|
|
% |
|
|
|
|
|||
2026 notes(4) |
|
|
|
% |
|
|
|
|
|||
2027 notes(4) |
|
|
|
% |
|
|
|
|
|||
2028 notes(4) |
|
|
|
% |
|
|
|
|
|||
2029 notes(4) |
|
|
|
% |
|
|
|
|
|||
2031 notes(4) |
|
% |
|
|
|||||||
2033 notes(4)(6) |
|
% |
|
— |
|||||||
Subordinated debt(2) |
|
|
N/A |
|
— |
|
|
||||
Sterling term loan(4)(7) |
|
|
N/A |
|
— |
|
|
||||
2017 OP term loan(8) |
|
|
N/A |
|
— |
|
|
||||
OP term loan(8)(9) |
|
|
|
% |
|
|
|
— |
|||
Deferred financing costs – net |
|
|
|
|
|
( |
|
( |
|||
Discount – net |
|
|
|
|
|
( |
|
( |
|||
Total senior notes and other unsecured borrowings – net |
|
|
|
|
|
|
|
|
|||
Total unsecured borrowings – net |
|
|
|
|
|
|
|
|
|||
Total secured and unsecured borrowings – net(10)(11) |
|
|
|
|
$ |
|
$ |
|
|||
| (1) |
Reflects the weighted average annual contractual interest rate on the mortgages at December 31, 2021. Secured by real estate assets with a net carrying value of $ |
| (2) | Wholly owned subsidiaries of Omega OP are the obligor on these borrowings. |
| (3) | Borrowing is the debt of a consolidated joint venture. |
| (4) | Guaranteed by Omega OP. |
| (5) |
In March 2021, we used a portion of the proceeds from the |
| (6) |
We used the proceeds from this offering to pay down outstanding borrowings on the 2017 Revolving Credit Facility, repay the Sterling term loan, and fund the tender offer to purchase $ |
| (7) |
Actual borrowing is in GBP and remeasured to USD. The Sterling term loan was settled in March 2021 using proceeds from the |
| (8) | Omega OP is the obligor on this borrowing. |
| (9) |
The weighted average interest rate of the OP Term Loan has been adjusted to reflect the impact of the interest rate swaps that effectively fix the LIBOR based portion of the interest rate at |
| (10) | All borrowings are direct borrowings of Parent unless otherwise noted. |
| (11) |
Certain of our other secured and unsecured borrowings are subject to customary affirmative and negative covenants, including financial covenants. |
F-44
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Secured Borrowings
HUD Mortgage Debt
On October 31, 2019, we assumed approximately $
On August 26, 2020, we paid approximately $
All HUD loans are subject to the regulatory agreements that require escrow reserve funds to be deposited with the loan servicer for mortgage insurance premiums, property taxes, debt service and capital replacement expenditures. As of December 31, 2021, the Company has total escrow reserves of $
Unsecured Borrowings
Revolving Credit Facility
On April 30, 2021, Omega entered into a credit agreement (the “2021 Omega Credit Agreement”) providing us with a new $
The Revolving Credit Facility bears interest at
We incurred $
F-45
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
OP Term Loan
On April 30, 2021, Omega OP entered into a credit agreement (the “2021 Omega OP Credit Agreement”) providing it with a new $
We incurred $
2017 Omega Credit Facilities
On May 25, 2017, Omega entered into a credit agreement (the “2017 Omega Credit Agreement”) for a new $
In 2020, we repaid the outstanding balance on our U.S. Term Loan and wrote-off $
2017 OP Term Loan
On May 25, 2017, Omega OP entered into a credit agreement (the “2017 Omega OP Credit Agreement”) providing it with a new $
Amended 2015 Term Loan Facility
On May 25, 2017, Omega entered into an amended and restated credit agreement (the “Amended 2015 Credit Agreement”), which amended and restated our previous $
Subordinated Debt
In connection with a 2010 acquisition, we assumed
F-46
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
General
The required principal payments, excluding the premium or discount and deferred financing costs on our secured and unsecured borrowings, for each of the five years following December 31, 2021 and the aggregate due thereafter are set forth below:
|
(in thousands) |
||
2022 |
|
$ |
|
2023 |
|
|
|
2024 |
|
|
|
2025 |
|
|
|
2026 |
|
|
|
Thereafter |
|
|
|
Total |
$ |
|
|
NOTE 15 – DERIVATIVES AND HEDGING
Cash Flow Hedges of Interest Rate Risk
We enter into interest rate swaps in order to maintain a capital structure containing targeted amounts of fixed and floating-rate debt and manage interest rate risk. Interest rate swaps designated as cash flow hedges involve the receipt of variable amounts from a counterparty in exchange for our fixed-rate payments. These interest rate swap agreements are used to hedge the variable cash flows associated with variable-rate debt.
As a result of exposure to interest rate movements associated with the Amended 2015 Term Loan Facility, on December 16, 2015, we entered into various forward-starting interest rate swap arrangements, which effectively converted $
On
F-47
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
In addition to the forward swaps discussed above, we also assumed various interest rate swap contracts in connection with the MedEquities Merger on May 17, 2019. We designated the interest rate swap contracts as cash flow hedges of interest rate risk associated with the 2017 Omega OP Credit Agreement. The assumed interest rate swap contracts effectively converted $
Foreign Currency Forward Contracts and Debt Designated as Net Investment Hedges
We use debt denominated in GBP and foreign currency forward contracts to hedge a portion of our net investment in the U.K. against fluctuations in foreign exchange rates.
GBP denominated borrowings under the Sterling term loan and the 2017 Revolving Credit Facility, were previously used to hedge a portion of our investments in the U.K. against fluctuations in GBP against the USD. The GBP denominated borrowings under both debt instruments were deemed an effective hedge from issuance in May 2017 until the settlement of the Sterling term loan and the repayment of the GBP denominated borrowings under the 2017 Revolving Credit Facility in March 2021.
Concurrent with the settlement of the GBP denominated debt, we entered into
The location and the fair value of derivative instruments designated as hedges, at the respective balance sheet dates, were as follows:
December 31, |
December 31, |
||||
2021 |
|
2020 |
|||
Cash flow hedges: |
(in thousands) |
||||
Other assets |
$ |
|
$ |
|
|
Accrued expenses and other liabilities |
$ |
|
$ |
|
|
Net investment hedges: |
|||||
Other assets |
$ |
|
$ |
— |
|
The fair value of the interest rate swaps and foreign currency forwards is derived from observable market data such as yield curves and foreign exchange rates and represents a Level 2 measurement on the fair value hierarchy.
NOTE 16 - FINANCIAL INSTRUMENTS
The net carrying amount of cash and cash equivalents, restricted cash, contractual receivables, other assets and accrued expenses and other liabilities reported in the Consolidated Balance Sheets approximates fair value because of the short maturity of these instruments (Level 1).
F-48
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
At December 31, 2021 and 2020, the net carrying amounts and fair values of other financial instruments were as follows:
December 31, 2021 |
December 31, 2020 |
|||||||||||
|
Carrying |
|
Fair |
|
Carrying |
|
Fair |
|||||
|
Amount |
|
Value |
|
Amount |
|
Value |
|||||
(in thousands) |
||||||||||||
Assets: |
||||||||||||
Investments in direct financing leases – net |
$ |
|
$ |
|
|
$ |
|
$ |
|
|||
Mortgage notes receivable – net |
|
|
|
|
|
|||||||
Other investments – net |
|
|
|
|
|
|||||||
Total |
$ |
|
$ |
|
$ |
|
$ |
|
||||
Liabilities: |
|
|
|
|
|
|
|
|
||||
2017 Revolving credit facility |
$ |
— |
$ |
— |
|
$ |
|
$ |
|
|||
Revolving credit facility |
— |
— |
|
— |
— |
|||||||
Term loan |
|
|
|
|
||||||||
Sterling term loan |
|
|
|
|
|
|||||||
2017 OP term loan |
|
— |
— |
|
|
|||||||
OP Term loan |
|
|
|
— |
— |
|||||||
|
|
|
|
|
||||||||
|
|
|
|
|
||||||||
|
|
|
|
|
||||||||
|
|
|
|
|
||||||||
|
|
|
|
|
||||||||
|
|
|
|
|
||||||||
|
|
|
|
|||||||||
|
|
|
|
|||||||||
|
|
— |
— |
|||||||||
HUD mortgages – net |
|
|
|
|
||||||||
Subordinated debt – net |
|
— |
— |
|
|
|||||||
Total |
$ |
|
$ |
|
$ |
|
$ |
|
||||
Fair value estimates are subjective in nature and are dependent on a number of important assumptions, including estimates of future cash flows, risks, discount rates and relevant comparable market information associated with each financial instrument (see Note 2 – Summary of Significant Accounting Policies). The use of different market assumptions and estimation methodologies may have a material effect on the reported estimated fair value amounts.
The following methods and assumptions were used in estimating fair value disclosures for financial instruments.
| ● | Mortgage notes receivable: The fair value of the mortgage notes receivables are estimated using a discounted cash flow analysis, using interest rates being offered for similar loans to borrowers with similar credit ratings (Level 3). |
| ● | Other investments: Other investments are primarily comprised of notes receivable. The fair values of notes receivable are estimated using a discounted cash flow analysis, using interest rates being offered for similar loans to borrowers with similar credit ratings (Level 3). |
| ● | Revolving credit facility and OP term loan: The carrying amount of these approximate fair value because the borrowings are interest rate adjusted. Differences between carrying value and the fair value in the table above are due to the inclusion of deferred financing costs in the carrying value. |
| ● | Senior notes: The fair value of the senior unsecured notes payable was estimated based on (Level 1) publicly available trading prices. |
F-49
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
| ● | Subordinated debt: The fair value of our borrowings under fixed rate agreements are estimated using a present value technique based on inputs from trading activity provided by a third party (Level 2). |
| ● | HUD mortgages: The fair value of our borrowings under HUD debt agreements are estimated using an expected present value technique based on quotes obtained by HUD debt brokers (Level 2). |
NOTE 17 – TAXES
Omega and Omega OP, including their wholly-owned subsidiaries were organized, have operated, and intend to continue to operate in a manner that enables Omega to qualify for taxation as a REIT under Sections 856 through 860 of the Code. On a quarterly and annual basis we perform several analyses to test our compliance within the REIT taxation rules. If we fail to meet the requirements for qualification as a REIT in any tax year, we will be subject to federal income tax on our taxable income at regular corporate rates and may not be able to qualify as a REIT for the subsequent years, unless we qualify for certain relief provisions that are available in the event we fail to satisfy any of the requirements.
We are also subject to federal taxation of
As a REIT under the Code, we generally will not be subject to federal income taxes on the REIT taxable income that we distribute to stockholders, subject to certain exceptions. In 2020, 2019, and 2018, we distributed dividends in excess of our taxable income.
We currently own stock in certain subsidiary REITs. These subsidiary entities are required to individually satisfy all of the rules for qualification as a REIT. If we fail to meet the requirements for qualification as a REIT for any of the subsidiary REITs, it may cause the Parent REIT to fail the requirements for qualification as a REIT also.
We have elected to treat certain of our active subsidiaries as TRSs. Our domestic TRSs are subject to federal, state and local income taxes at the applicable corporate rates. Our foreign TRSs are subject to foreign income taxes and may be subject to current-year income inclusion relating to ownership of a controlled foreign corporation for U.S. income tax purposes. As of December 31, 2021,
The following is a summary of our provision for income taxes:
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
2018 |
|||||
(in millions) |
|||||||||
Provision for federal, state and local income taxes |
$ |
|
$ |
|
$ |
|
|||
Provision for foreign income taxes |
|
|
|
||||||
Total provision for income taxes (1) |
$ |
|
$ |
|
$ |
|
|||
| (1) | The above amounts do not include gross income receipts or franchise taxes payable to certain states and municipalities. |
F-50
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
The following is a summary of deferred tax assets and liabilities:
December 31, |
December 31, |
|||||
|
2021 |
|
2020 |
|||
(in thousands) |
||||||
Deferred tax assets: |
|
|
|
|
||
Federal net operating loss carryforward |
$ |
|
$ |
|
||
Deferred tax liability: |
|
|
|
|
||
Foreign deferred tax liability (1) |
|
( |
|
( |
||
Valuation allowance on deferred tax asset |
|
( |
|
( |
||
Net deferred tax liability |
$ |
( |
$ |
( |
||
| (1) | The deferred tax liability primarily resulted from inherited basis differences resulting from our acquisition of entities in the U.K. Subsequent adjustments to these accounts result from GAAP to tax differences related to depreciation, indexation and revenue recognition. |
NOTE 18 – STOCKHOLDERS’ EQUITY
$300 Million 2019 Forward Equity Sale
In connection with a $
$
On March 20, 2020, Omega’s Board of Directors authorized the repurchase of up to $
At-The-Market Offering Program
On September 3, 2015, we entered into separate Equity Distribution Agreements with several financial institutions to sell $
During the second quarter of 2021, we terminated the 2015 ATM Program and entered into a new ATM Equity Offering Sales Agreement pursuant to which shares of common stock having an aggregate gross sales price of up to $
F-51
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
The following is a summary of the shares issued under the 2021 and 2015 ATM Programs for each of the years ended December 31, 2019, 2020, and 2021 (in millions except average price per share):
Average Net Price |
|||||||||
Year Ended |
Shares issued |
Per Share(1) |
Gross Proceeds |
Commissions |
Net Proceeds |
||||
December 31, 2019 |
|
$ |
|
$ |
|
$ |
|
$ |
|
December 31, 2020 |
|
|
|
|
|
||||
December 31, 2021 |
|
|
|
|
|
||||
| (1) | Represents the average price per share after commissions. |
Dividend Reinvestment and Common Stock Purchase Plan
We have a Dividend Reinvestment and Common Stock Purchase Plan (the “DRSPP”) that allows for the reinvestment of dividends and the optional purchase of our common stock. On March 23, 2020, we temporarily suspended the DRSPP and on December 17, 2020, we reinstated the DRSPP. The table below presents information regarding the shares issued under the DRSPP for each of the years ended December 31, 2019, 2020, and 2021 (in millions):
Year Ended |
Shares issued |
Gross Proceeds |
|
December 31, 2019 |
|
$ |
|
December 31, 2020 |
|
|
|
December 31, 2021 |
|
|
|
Dividends
The Board of Directors has declared common stock dividends as set forth below:
Record |
Payment |
Dividend per |
|||
Date |
|
Date |
|
Common Share |
|
$ |
|||||
Per Share Distributions
Per share distributions by our Company were characterized in the following manner for income tax purposes (unaudited):
Year Ended December 31, |
|||||||||
Common |
|
2021 |
|
2020 |
|
2019 |
|||
Ordinary income |
$ |
|
$ |
|
$ |
|
|||
Return of capital |
|
|
|
|
|
|
|||
Capital gains |
|
|
|
|
|
|
|||
Total dividends paid |
$ |
|
$ |
|
$ |
|
|||
For additional information regarding dividends, see Note 17 – Taxes.
F-52
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Accumulated Other Comprehensive Income (Loss)
The following is a summary of our accumulated other comprehensive income (loss), net of tax where applicable:
As of and for the |
|||||||||
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
|
2019 |
||||
(in thousands) |
|||||||||
Foreign Currency Translation: |
|
|
|
|
|
||||
Beginning balance |
$ |
( |
$ |
( |
$ |
( |
|||
Translation (loss) gain |
|
( |
|
|
|
|
|||
Realized gain (loss) |
|
|
|
|
|
( |
|||
Ending balance |
|
( |
|
( |
|
( |
|||
Derivative Instruments: |
|
|
|
|
|
|
|||
Cash flow hedges: |
|
|
|
|
|
|
|||
Beginning balance |
|
|
|
( |
|
|
|||
Unrealized gain (loss) |
|
|
|
|
|
( |
|||
Realized gain (loss)(1) |
|
|
|
( |
|
|
|||
Ending balance |
|
|
|
|
|
( |
|||
Net investment hedges: |
|
|
|
|
|
|
|||
Beginning balance |
|
( |
|
( |
|
|
|||
Unrealized gain (loss) |
|
|
|
( |
|
( |
|||
Ending balance |
|
( |
|
( |
|
( |
|||
Total accumulated other comprehensive loss before noncontrolling interest |
|
( |
|
( |
|
( |
|||
Add: portion included in noncontrolling interest |
|
|
|
|
|
|
|||
Total accumulated other comprehensive loss for Omega |
$ |
( |
$ |
( |
$ |
( |
|||
(1) |
Expenses related to our effective cash flow hedges are recorded within interest expense. As noted in Note 15 – Derivatives and Hedging, we terminated $ |
NOTE 19 – STOCK-BASED COMPENSATION
At December 31, 2021, we maintained several stock-based compensation plans as described below. For the years ended December 31, 2021, 2020 and 2019, we recognized stock-based compensation of $
Time-Based Restricted Equity Awards
Restricted stock, restricted stock units (“RSUs”) and profits interest units (“PIUs”) are subject to forfeiture if the holder’s service to us terminates prior to vesting, subject to certain exceptions for certain qualifying terminations of service or a change in control of the Company. Prior to vesting, ownership of the shares/units cannot be transferred. The restricted stock has the same dividend and voting rights as our common stock. RSUs accrue dividend equivalents but have no voting rights. PIUs accrue distributions, which are equivalent to dividend equivalents, but have no voting rights. Once vested, each RSU is settled by the issuance of
F-53
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Performance-Based Restricted Equity Awards
Performance-based restricted equity awards include performance restricted stock units (“PRSUs”) and PIUs. PRSUs and PIUs are subject to forfeiture if the performance requirements are not achieved or if the holder’s service to us terminates prior to vesting, subject to certain exceptions for certain qualifying terminations of employment or a change in control of the Company. PRSUs and PIUs have varying degrees of performance requirements to achieve vesting, and each PRSU and PIU award represents the right to a variable number of shares of common stock or partnership units. Each PIU once earned is convertible into
Prior to vesting and the distribution of shares or Omega OP Units, ownership of the PRSUs or PIUs cannot be transferred. Dividend equivalents on the PRSUs are accrued and paid to the extent the applicable performance requirements are met. While each PIU is unearned, the employee receives a partnership distribution equal to
January 1, |
January 1, |
January 1, |
|
||||||||||||||||
|
2021 |
|
2020 |
2019 |
|
||||||||||||||
Closing price on date of grant |
$ |
|
$ |
|
$ |
|
|||||||||||||
Dividend yield |
|
|
% |
|
% |
|
% |
||||||||||||
Risk free interest rate at time of grant |
|
|
% |
to |
|
% |
|
% |
to |
|
% |
|
% |
to |
|
% |
|||
Expected volatility |
|
|
% |
to |
|
% |
|
% |
to |
|
% |
|
% |
to |
|
% |
|||
The following table summarizes the activity in restricted stock, RSUs, PRSUs, and PIUs for the years ended December 31, 2019, 2020 and 2021:
Time-Based |
Performance-Based |
||||||||||||
|
|
|
Weighted - |
|
|
Weighted - |
|
Total |
|||||
Number of |
Average Grant- |
Number of |
Average Grant- |
Compensation |
|||||||||
Shares/Omega |
Date Fair Value |
Shares/Omega |
Date Fair Value |
Cost (1) |
|||||||||
|
OP Units |
|
per Share |
OP Units |
|
per Share |
|
(in millions) |
|||||
Non-vested at December 31, 2018 |
|
|
|
|
|
|
|||||||
Granted during 2019 |
|
|
|
|
|
|
|
$ |
|
||||
Cancelled during 2019 |
|
( |
|
|
( |
|
|
|
|
||||
Vested during 2019 |
|
( |
|
|
( |
|
|
|
|
||||
Non-vested at December 31, 2019 |
|
|
|
|
|
|
|
||||||
Granted during 2020 |
|
|
|
|
|
|
|
$ |
|
||||
Cancelled during 2020 |
|
( |
|
|
( |
|
|
|
|
||||
Vested during 2020 |
|
( |
|
|
( |
|
|
|
|
||||
Non-vested at December 31, 2020 |
|
|
|
|
|
|
|
||||||
Granted during 2021 |
|
|
|
|
|
|
|
$ |
|
||||
Cancelled during 2021 |
|
( |
|
|
( |
|
|
|
|
||||
Forfeited during 2021 |
|
— |
|
— |
( |
|
|
|
|
||||
Vested during 2021 (2) |
|
( |
|
|
( |
|
|
|
|
||||
Non-vested at December 31, 2021 |
|
|
$ |
|
|
$ |
|
|
|
||||
(1) |
Total compensation cost to be recognized on the awards based on grant date fair value. |
(2) |
PRSUs are shown as vesting in the year that the Compensation Committee determines the level of achievement of the applicable performance measures. |
F-54
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
As of December 31, 2021, unrecognized compensation costs related to unvested awards to employees is as follows:
| ● |
$ |
| ● |
$ |
| ● |
$ |
| ● |
$ |
In addition, we have a deferred stock compensation plan that allows employees and directors the ability to defer the receipt of stock awards (units). The deferred stock awards (units) participate in future dividend equivalents as well as the change in the value of the Company’s common stock. As of December 31, 2021 and 2020, the Company had
Tax Withholding for Stock Compensation Plans
Stock withheld to pay tax withholdings for equity instruments granted under stock-based payment arrangements for the years ended December 31, 2021, 2020 and 2019, was $
Shares Available for Issuance for Compensation Purposes
On June 8, 2018, at the Annual Meeting of Stockholders, our stockholders approved the 2018 Stock Incentive Plan (the “2018 Plan”), which amended and restated the Company’s 2013 Stock Incentive Plan (the “2013 Plan”). The 2018 Plan is a comprehensive incentive compensation plan that allows for various types of equity-based compensation, including RSUs (including PRSUs), stock awards (including restricted stock), deferred RSUs, incentive stock options, non-qualified stock options, stock appreciation rights, dividend equivalent rights, performance unit awards, certain cash-based awards (including performance-based cash awards), PIUs and other stock-based awards. The 2018 Plan increased the number of shares of common stock available for issuance under the 2013 Plan by
As of December 31, 2021, approximately
F-55
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
NOTE 20 – COMMITMENTS AND CONTINGENCIES
Shareholder Litigation
The Company and certain of its officers, C. Taylor Pickett, Robert O. Stephenson, and Daniel J. Booth, are defendants in a purported securities class action lawsuit pending in the U.S. District Court for the Southern District of New York (the “Securities Class Action”). Brought by lead plaintiff Royce Setzer and additional plaintiff Earl Holtzman, the Securities Class Action purports to assert claims for violations of Section 10(b) of the Securities Exchange Act of 1934, as amended (the “Exchange Act”) and Rule 10b-5 promulgated thereunder, as well as Section 20(a) of the Exchange Act, and seeks an unspecified amount of monetary damages, interest, fees and expenses of attorneys and experts, and other relief. The Securities Class Action alleges that the defendants violated the Exchange Act by making materially false and/or misleading statements, and by failing to disclose material adverse facts about the Company’s business, operations, and prospects, including the financial and operating results of one of the Company’s operators, the ability of such operator to make timely rent payments, and the impairment of certain of the Company’s leases and the uncollectibility of certain receivables. The initial complaint was dismissed with prejudice by the U.S District Court, but the dismissal was overturned by the U.S Court of Appeals for the Second Circuit in 2020. Thereafter, the plaintiffs filed a Second Consolidated Amended Complaint in August 2020. In November 2020, the Company and the officers named in the Securities Class Action filed a Motion to Dismiss the Second Consolidated Amended Complaint. On September 28, 2021, the Court issued an order denying the motion to dismiss insofar as it requested dismissal of the entire action on grounds of loss causation, and granting it insofar as it sought dismissal of any claims arising out of defendants’ statements in February 2017. Because the dismissed claims were the basis for defendants’ efforts to begin the alleged class period in February 2017, the decision means that the alleged class period runs from May 3, 2017 to October 31, 2017.
Certain derivative actions have also been brought against the officers named in the Securities Class Action, and certain current and former directors of the Company, alleging claims relating to the matters at issue in the Securities Class Action. These derivative actions are currently stayed pending certain developments in the Securities Class Action.
In 2018, Stourbridge Investments LLC, a purported stockholder of the Company, filed a derivative action purportedly on behalf of the Company in the U.S. District Court for the Southern District of New York, alleging violations of Section 14(a) of the Exchange Act and state-law claims including breach of fiduciary duty. The complaint alleges, among other things, that the named defendants are responsible for the Company’s failure to disclose the financial condition of Orianna Health Systems, the alleged non-disclosures that are also the subject of the Securities Class Action described above. The plaintiff did not make a demand on the Company to bring the action prior to filing it, but rather alleges that demand would have been futile. The case has been stayed pending the entry of judgment or a voluntary dismissal with prejudice in the Securities Class Action.
In 2019, purported stockholder Phillip Swan by his counsel, and stockholders Tom Bradley and Sarah Smith by their counsel, filed derivative actions in the Baltimore City Circuit Court of Maryland, purportedly on behalf of the Company, asserting claims for breach of fiduciary duty, waste of corporate assets and unjust enrichment against the named defendants. Those actions have been consolidated and stayed in the Maryland court pending completion of fact discovery in the Securities Class Action. Prior to filing suit, each of these stockholders had made demands on the Board of Directors in 2018 that the Company bring such lawsuits. After an investigation and due consideration, and in the exercise of its business judgment, the Board of Directors determined that it is not in the best interests of the Company to commence litigation against any current or former officers or directors based on the matters raised in the demands.
In addition, in late 2020, Robert Wojcik, a purported shareholder of the Company, filed a derivative action in the U.S. District Court for the District of Maryland, purportedly on behalf of the Company, asserting violations of Section 14(a) of the Exchange Act, Sections 10(b) and 21D of the Exchange Act, as well as claims for breach of fiduciary duty, unjust enrichment, abuse of control, gross mismanagement, and waste of corporate assets. Wojcik also did not make a demand on the Company prior to filing suit. The case has been stayed pending the entry of judgment or a voluntary dismissal with prejudice in the Securities Class Action.
The Company believes that the claims asserted against it in these lawsuits are without merit and intends to vigorously defend against them.
F-56
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Other
Gulf Coast Subordinated Debt
In August 2021, we filed suit in the Circuit Court for Baltimore County against the holders of certain Subordinated Debt associated with our Gulf Coast master lease agreement, following an assertion by the holders that our prior exercise of offset rights in connection with Gulf Coast’s non-payment of rent had resulted in defaults under the terms of the Subordinated Debt. The suit seeks a declaratory judgment to, among other items, declare that the aggregate amount of unpaid rent due from Gulf Coast under the master lease agreement exceeds all amounts which otherwise would be due and owing by Omega Obligor under the Subordinated Debt, and that all principal and interest due and owing under the Subordinated Debt may be (and was) offset in full as of December 31, 2021. In October 2021, the defendants in the case filed a motion to dismiss for lack of personal jurisdiction, with a hearing scheduled on the motion for February 25, 2022. While Omega believes Omega Obligor is entitled to the enforcement of the offset rights sought in the action, the outcome of litigation is unpredictable, and Omega cannot predict the outcome of the declaratory judgment action. See Note 5 – Contractual Receivables and Other Receivables and Lease Inducements – Gulf Coast Health Care, LLC.
Lakeway Realty, L.L.C.
In September 2016, MedEquities received a Civil Investigative Demand (“CID”) from the U.S. Department of Justice (“DOJ”), which indicates that it is conducting an investigation regarding alleged violations of the False Claims Act, Stark Law and Anti-Kickback Statute in connection with claims that may have been submitted to Medicare and other federal payors for services rendered to patients at Lakeway Hospital or by providers with financial relationships with Lakeway Hospital. As a result of the acquisition of MedEquities, the Company owns a
On September 29, 2020 the DOJ announced it had reached a settlement of a False Claims Act case with respect to certain aspects of the investigation with Lakeway Regional Medical Center wherein Lakeway Regional Medical Center agreed to pay $
The Company believes that the acquisition, ownership and leasing of Lakeway Hospital through the Lakeway Partnership was and is in compliance with all applicable laws. However, due to the uncertainties surrounding this matter and its ultimate outcome, we are unable to determine whether it is probable that any loss has been incurred.
In addition, we are subject to various other legal proceedings, claims and other actions arising out of the normal course of business. While any legal proceeding or claim has an element of uncertainty, management believes that the outcome of each lawsuit, claim or legal proceeding that is pending or threatened, or all of them combined, will not have a material adverse effect on our consolidated financial position or results of operations.
Indemnification Agreements
In connection with certain facility transitions, we have agreed to indemnify certain operators in certain events. As of December 31, 2021, our maximum funding commitment under these indemnification agreements was approximately $
F-57
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
Commitments
We have committed to fund the construction of new leased and mortgaged facilities, capital improvements and other commitments. We expect the funding of these commitments to be completed over the next several years.
Total commitments (1) |
|
$ |
|
||
Amounts funded to date (2) |
|
( |
|||
Remaining commitments (3) |
$ |
|
|||
| (1) |
Includes our $ |
| (2) | Includes finance costs. |
| (3) |
This amount excludes our remaining commitments to fund under our other investments of approximately $ |
Environmental Matters
As of December 31, 2021 and 2020, we had identified conditional asset retirement obligations primarily related to the future removal and disposal of asbestos that is contained within certain of our real estate investment properties. The asbestos is appropriately contained, and we believe we are compliant with current environmental regulations. If these properties undergo major renovations or are demolished, certain environmental regulations are in place, which specify the manner in which asbestos must be handled and disposed. We are required to record the fair value of these conditional liabilities if they can be reasonably estimated. As of December 31, 2021 and 2020,
F-58
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
NOTE 21 – SUPPLEMENTAL DISCLOSURE TO CONSOLIDATED STATEMENTS OF CASH FLOWS
The following are supplemental disclosures to the consolidated statements of cash flows for the years ended December 31, 2021, 2020 and 2019:
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
|
2019 |
||||
|
(in thousands) |
||||||||
Reconciliation of cash and cash equivalents and restricted cash: |
|||||||||
Cash and cash equivalents |
$ |
|
|
$ |
|
|
$ |
|
|
Restricted cash |
|
|
|
|
|
|
|||
Cash, cash equivalents and restricted cash at end of year |
$ |
|
$ |
|
$ |
|
|||
Supplemental information: |
|
|
|
|
|
|
|||
Interest paid during the year, net of amounts capitalized |
$ |
|
$ |
|
$ |
|
|||
Taxes paid during the year |
$ |
|
$ |
|
$ |
|
|||
Non cash investing activities |
|
|
|
|
|
|
|||
Non-cash acquisition of business |
$ |
|
$ |
( |
$ |
( |
|||
Non-cash acquisition of real estate |
$ |
( |
$ |
|
$ |
( |
|||
Non-cash proceeds from sale of real estate investments |
$ |
|
$ |
|
$ |
|
|||
Non-cash placement of mortgage principal |
$ |
( |
$ |
( |
$ |
|
|||
Non-cash collection of mortgage principal |
$ |
|
$ |
|
$ |
|
|||
Non-cash surrender of mortgage |
$ |
|
$ |
|
$ |
|
|||
Non-cash investment in other investments |
$ |
|
$ |
( |
$ |
( |
|||
Non-cash proceeds from other investments |
$ |
|
$ |
|
$ |
|
|||
Non-cash settlement of direct financing lease |
$ |
|
$ |
|
$ |
|
|||
Initial non-cash right of use asset - ground leases |
$ |
|
$ |
|
$ |
|
|||
Initial non-cash lease liability - ground leases |
$ |
|
$ |
|
$ |
( |
|||
Non cash financing activities |
|
|
|
||||||
Debt assumed in merger |
$ |
|
$ |
|
$ |
|
|||
Stock exchanged in merger |
$ |
|
$ |
|
$ |
|
|||
Acquisition of other long-term borrowings |
$ |
|
$ |
|
$ |
|
|||
Non-cash borrowing (repayment) of other long-term borrowings |
$ |
( |
$ |
|
$ |
( |
|||
Change in fair value of cash flow hedges |
$ |
|
$ |
|
$ |
( |
|||
Remeasurement of debt denominated in a foreign currency |
$ |
|
$ |
|
$ |
|
|||
F-59
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
NOTE 22 - EARNINGS PER SHARE
The following tables set forth the computation of basic and diluted earnings per share:
Year Ended December 31, |
|||||||||
|
2021 |
|
2020 |
|
2019 |
||||
(in thousands, except per share amounts) |
|||||||||
Numerator: |
|
|
|
|
|
||||
Net income |
$ |
|
$ |
|
$ |
|
|||
Deduct: net income attributable to noncontrolling interests |
|
( |
|
( |
|
( |
|||
Net income available to common stockholders |
$ |
|
$ |
|
$ |
|
|||
Denominator: |
|
|
|
|
|
|
|||
Denominator for basic earnings per share |
|
|
|
|
|
|
|||
Effect of dilutive securities: |
|
|
|
|
|
|
|||
Common stock equivalents |
|
|
|
|
|
|
|||
Net forward share contract |
— |
— |
|
||||||
Noncontrolling interest – Omega OP Units |
|
|
|
|
|
|
|||
Denominator for diluted earnings per share |
|
|
|
|
|
|
|||
Earnings per share - basic: |
|
|
|
|
|
|
|||
Net income available to common stockholders |
$ |
|
$ |
|
$ |
|
|||
Earnings per share – diluted: |
|
|
|
|
|
|
|||
Net income |
$ |
|
$ |
|
$ |
|
|||
In September 2019, we entered into a forward equity sales agreement to sell up to an aggregate of
NOTE 23 – SUBSEQUENT EVENTS
Asset Acquisitions
On January 1, 2022, we a Maryland SNF for $
On January 31, 2022, we acquired
F-60
OMEGA HEALTHCARE INVESTORS, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS – Continued
$500 Million Stock Repurchase Program
On January 27, 2022, the Company authorized the repurchase of up to $
Operator Collectibility
In January and February 2022, an operator representing
As discussed in Note 8 – Other Investments under “Revolving Credit Facility - $
Guardian
In connection with on-going restructuring negotiations with Guardian, in February 2022, we completed the sale of
On February 15, 2022, Guardian completed the sale of
Guardian failed to make rent and interest payments in January and February 2022 and discussions on restructuring the remaining Guardian lease facilities are on-going.
F-61
SCHEDULE II – VALUATION AND QUALIFYING ACCOUNTS
(in thousands)
|
Balance at |
|
Charged to |
|
|
|
Balance at |
|||||
Beginning of |
Provision |
Deductions or |
End of |
|||||||||
Description |
Period |
Accounts |
Other (1) |
Period |
||||||||
Year Ended December 31, 2019: |
|
|
|
|
|
|
|
|
||||
Allowance for doubtful accounts: |
|
|
|
|
|
|
|
|
||||
Contractual receivables (2) |
$ |
|
$ |
— |
$ |
|
$ |
— |
||||
Mortgage notes receivable (3) |
|
|
|
— |
|
|
|
|
||||
Direct financing leases (3) |
|
|
|
|
|
|
|
|
||||
Total |
$ |
|
$ |
|
$ |
|
$ |
|
||||
| (1) | Uncollectible accounts written off, net of recoveries or adjustments. |
| (2) | The Company adopted Topic 842 on January 1, 2019. As a result of this adoption, lease related receivables are written off through rental income, as opposed to the provision account. As such, our lease receivables are no longer considered in the valuation and qualifying accounts. |
| (3) | The Company adopted Topic 326 on January 1, 2020 which addressed expected credit losses on our mortgage notes receivables, other investments, and direct financing leases. As a result of this adoption, we have disclosed a rollforward of our allowance for credit loss related to these financial instruments for 2020 and 2021 in Note 9 – Allowance for Credit Losses. |
F-62
OMEGA HEALTHCARE INVESTORS, INC.
SCHEDULE III – REAL ESTATE AND ACCUMULATED DEPRECIATION
(in thousands)
December 31, 2021
Gross Amount at |
|||||||||||||||||||||||||||||||||
Initial Cost to |
Cost Capitalized |
Which Carried at |
Life on Which |
||||||||||||||||||||||||||||||
Company |
Subsequent to |
Close of Period (3) (5) |
Depreciation |
||||||||||||||||||||||||||||||
Acquisition |
(4) |
(7) |
in Latest |
||||||||||||||||||||||||||||||
Buildings and |
Carrying |
(6) |
(8) |
Buildings and |
Accumulated |
Date of |
Date |
Income Statements |
|||||||||||||||||||||||||
Description (1) |
Encumbrances |
Land |
|
Improvements |
|
Improvements |
|
Cost |
|
Other |
|
Land |
|
Improvements |
|
Total |
|
Depreciation |
|
Construction |
|
Acquired |
|
is Computed |
|||||||||
Alabama (SNF) |
$ |
|
$ |
|
$ |
|
$ |
— |
$ |
— |
$ |
|
$ |
|
$ |
|
$ |
( |
|
|
|
||||||||||||
Arizona (ALF, SNF, ILF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Arkansas (ALF, SNF) |
|
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
|
|
|||||||||||
California (ALF, SH, SNF) |
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Colorado (ILF, SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Connecticut (ALF) |
|
|
|
|
|
|
|
|
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Florida (ALF, SNF, ILF) |
(2) |
|
|
|
|
|
|
|
|
|
( |
|
|
|
|
|
|
|
( |
|
|
|
|||||||||||
Georgia (ALF, SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Idaho (SNF) |
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
||||||||||||||
Illinois (ALF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
||||||||||||||
Indiana (ALF, ILF, IRF, MOB, SH, SNF) |
|
|
|
|
|
|
|
— |
|
|
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Iowa (SNF) |
|
|
|
|
|
— |
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Kansas (SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Kentucky (ALF, SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Louisiana (ALF, SNF) |
(2) |
|
|
|
|
|
|
|
|
|
( |
|
|
|
|
|
|
|
( |
|
|
|
|||||||||||
Maryland (SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Massachusetts (ALF, SNF) |
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Michigan (SNF) |
|
|
|
|
|
— |
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Minnesota (ALF, ILF, SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Mississippi (SNF) |
(2) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
|||||||||||
Missouri (SNF) |
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Montana (SNF) |
|
|
|
|
|
— |
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Nevada (BHS, SH, SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
New Hampshire (ALF, SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
New Jersey (ALF) |
|
|
|
|
|
|
|
|
|
— |
|
|
|
|
|
|
|
( |
|
||||||||||||||
New Mexico (SNF) |
|
|
|
— |
— |
|
|
|
( |
|
|
||||||||||||||||||||||
New York (ALF) |
|
|
— |
|
— |
|
|
|
( |
||||||||||||||||||||||||
North Carolina (SNF) |
(2) |
|
|
|
|
( |
|
|
|
( |
|
|
|||||||||||||||||||||
Ohio (BHP, BHS, ALF, SH, SNF) |
|
|
|
|
( |
|
|
|
( |
|
|
||||||||||||||||||||||
Oklahoma (SNF) |
|
|
— |
— |
— |
|
|
|
( |
|
|
||||||||||||||||||||||
Oregon (ALF, SNF, ILF) |
|
|
|
— |
— |
|
|
|
( |
|
|
||||||||||||||||||||||
Pennsylvania (ALF, ILF, SNF) |
|
|
|
— |
( |
|
|
|
( |
|
|
||||||||||||||||||||||
Rhode Island (SNF) |
|
|
|
— |
— |
|
|
|
( |
|
|
||||||||||||||||||||||
South Carolina (SNF) |
|
|
|
— |
— |
|
|
|
( |
|
|
||||||||||||||||||||||
Tennessee (ALF, BHP, SNF) |
|
|
|
— |
— |
|
|
|
( |
|
|
||||||||||||||||||||||
Texas (ALF, BHS, ILF, IRF, MOB, SH, SNF) |
|
|
|
|
|
|
|
|
|
( |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
United Kingdom (ALF) |
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Vermont (SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Virginia (ALF, SNF) |
|
|
|
— |
( |
|
|
|
( |
|
|
||||||||||||||||||||||
Washington (ALF, SNF) |
|
|
|
|
|
|
|
— |
|
( |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Washington DC (ALF) |
|
|
|
— |
|
|
|
|
|
— |
|
|
|
|
|
|
|
— |
|
N/A |
|||||||||||||
West Virginia (SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Wisconsin (SNF) |
|
|
|
|
|
|
|
— |
|
— |
|
|
|
|
|
|
|
( |
|
|
|
||||||||||||
Total |
$ |
|
$ |
|
$ |
|
$ |
|
$ |
( |
$ |
|
$ |
|
$ |
|
$ |
( |
|
|
|
|
|
|
|||||||||
| (1) | The real estate included in this schedule is being used in either the operation of skilled nursing facilities (“SNF”), assisted living facilities (“ALF”), independent living facilities (“ILF”), specialty facilities (consisting of behavioral health substance facilities (“BHS”), behavioral health psychology facilities (“BHP”), independent rehabilitation facilities (“IRF”) and specialty hospitals (“SH”)) or medical office buildings (“MOB”), located in the states or country indicated. |
| (2) |
Certain of the real estate indicated are security for the HUD loan borrowings totaling $ |
F-63
OMEGA HEALTHCARE INVESTORS, INC.
SCHEDULE III – REAL ESTATE AND ACCUMULATED DEPRECIATION — continued
(in thousands)
December 31, 2021
(3)
Year Ended December 31, |
|||||||||
|
2019 |
|
2020 |
|
2021 |
||||
Balance at beginning of period |
$ |
|
$ |
|
$ |
|
|||
Acquisitions through foreclosure |
|
|
|
— |
|
||||
Acquisitions (a) |
|
|
|
|
|
|
|||
Impairment |
|
( |
|
( |
|
( |
|||
Improvements |
|
|
|
|
|
|
|||
Disposals/other |
|
( |
|
( |
|
( |
|||
Balance at close of period |
$ |
|
$ |
|
$ |
|
|||
| (a) |
Includes approximately $ |
(4)
Year Ended December 31, |
|||||||||
|
2019 |
|
2020 |
|
2021 |
||||
Balance at beginning of period |
$ |
|
$ |
|
$ |
|
|||
Provisions for depreciation |
|
|
|
|
|
|
|||
Dispositions/other |
|
( |
|
( |
|
( |
|||
Balance at close of period |
$ |
|
$ |
|
$ |
|
|||
(5) The reported amount of our real estate at December 31, 2021 is greater than the tax basis of the real estate by approximately $
(6) Reflects bed sales, impairments (including the write-off of accumulated depreciation), land easements and impacts from foreign currency exchange rates.
(7) To the extent that we acquired an entity previously owning the underlying facility, the acquisition date reflects the date that the entity acquired the facility.
(8) Includes $
F-64
SCHEDULE IV – MORTGAGE LOANS ON REAL ESTATE
(in thousands)
December 31, 2021
Carrying |
|
|||||||||||||||||||||
Amount of |
|
|||||||||||||||||||||
Carrying |
Loans |
|
||||||||||||||||||||
Face |
Amount |
Subject to |
|
|||||||||||||||||||
Final |
Amount |
of |
Delinquent |
|
||||||||||||||||||
Interest |
Fixed/ |
Maturity |
Prior |
of |
Mortgages |
Principal |
|
|||||||||||||||
Grouping |
|
Description (1) |
|
Rate |
|
Variable |
|
Date |
|
Periodic Payment Terms |
|
Liens |
|
Mortgages |
|
(3) (4) (6) |
|
or Interest |
|
|||
First Mortgages |
||||||||||||||||||||||
1 |
|
Michigan (25 SNFs) |
|
|
% |
|
|
|
$ |
|
$ |
|
$ |
— |
||||||||
2 |
|
Michigan (5 SNFs) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
3 |
|
Michigan (2 SNFs) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
4 |
|
Ohio (8 SNFs) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
5 |
|
Ohio (2 SNFs) and Pennsylvania (4 SNFs and 1 ALFs) |
|
|
% |
|
|
|
|
|
|
|
|
|
(5) |
|||||||
6 |
|
Texas (1 specialty facility) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
7 |
|
Massachusetts (1 specialty facility) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
8 |
|
Tennessee ( 1 SNF) |
|
|
% |
|
|
|
|
|
|
|
|
|
(5) |
|||||||
9 |
Michigan (1 SNF) |
|
% |
|
|
— |
||||||||||||||||
10 |
|
Michigan (1 SNF) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
11 |
Ohio (1 SNF) |
|
% |
|
|
— |
||||||||||||||||
12 |
Michigan (8 SNFs and 1 ALF) |
|
% |
|
|
— |
||||||||||||||||
13 |
Michigan (1 SNF) |
|
% |
|
|
|||||||||||||||||
Capital Expenditure Mortgages |
||||||||||||||||||||||
14 |
|
Michigan |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
15 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
16 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
17 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
18 |
|
Michigan |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
19 |
|
Michigan |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
20 |
|
Michigan |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
21 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
22 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
23 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
24 |
Michigan |
|
% |
|
|
— |
||||||||||||||||
Construction Mortgages |
||||||||||||||||||||||
25 |
|
Michigan (1 SNF) |
|
|
% |
|
|
|
|
|
|
|
|
— |
||||||||
Allowance for credit loss on mortgage loans(7) |
— |
( |
— |
|||||||||||||||||||
|
|
|
|
|
|
$ |
|
$ |
|
$ |
|
|||||||||||
| (1) | Loans included in this schedule represent first mortgages, capital expenditure mortgages and construction mortgages on facilities used in the delivery of long-term healthcare of which such facilities are located in the states indicated. |
| (2) | Interest on the loans escalates annually at a fixed rate. |
| (3) |
The aggregate cost for federal income tax purposes is approximately $ |
F-65
OMEGA HEALTHCARE INVESTORS, INC.
SCHEDULE IV – MORTGAGE LOANS ON REAL ESTATE — continued
(in thousands)
December 31, 2021
(4)
Year Ended December 31, |
|||||||||
|
2019 |
|
2020 |
|
2021 |
||||
Balance at beginning of period |
$ |
|
$ |
|
$ |
|
|||
Additions during period - new mortgage loans or additional fundings (a) |
|
|
|
|
|
|
|||
Deductions during period - collection of principal/other (b) |
|
( |
|
( |
|
( |
|||
Allowance for credit loss on mortgage loans |
|
— |
|
( |
|
( |
|||
Balance at close of period |
$ |
|
$ |
|
$ |
|
|||
| (a) |
The 2019 amount includes $ |
| (b) |
The 2019 amount includes $ |
| (7) | The allowance for credit loss on mortgage loans represents the allowance calculated utilizing a PD and LGD methodology. For mortgages that the risk of loss was evaluated on an individual basis, the allowance is included as a reduction to the carrying amount of the mortgage. |
F-66
INDEX TO EXHIBITS TO 2021 FORM 10-K
EXHIBIT NUMBER |
DESCRIPTION |
2.1 |
|
3.1 |
|
3.2 |
|
3.3 |
|
3.4 |
|
3.5 |
|
4.0 |
See Exhibits 3.1 to 3.5. |
4.1 |
|
4.1A |
|
4.1B |
|
4.1C |
|
4.1D |
|
4.1E |
|
4.1F |
I-1
4.1G |
|
4.1H |
|
4.1I |
|
4.1J |
|
4.1K |
|
4.1L |
|
4.1M |
|
4.2 |
|
4.2A |
|
4.2B |
|
4.2C |
|
4.2D |
|
4.2E |
|
4.2F |
|
4.2G |
I-2
4.2H |
|
4.2I |
|
4.2J |
|
4.2K |
|
4.2L |
|
4.3 |
|
4.3A |
|
4.3B |
|
4.3C |
|
4.3D |
|
4.3E |
|
4.3F |
|
4.3G |
|
4.3H |
|
4.3I |
I-3
4.3J |
|
4.4 |
|
4.4A |
|
4.4B |
|
4.4C |
|
4.4D |
|
4.4E |
|
4.4F |
|
4.4G |
|
4.4H |
|
4.5 |
|
4.5A |
|
4.5B |
|
4.5C |
|
4.5D |
I-4
4.5E |
|
4.6 |
|
4.6A |
|
4.6B |
|
4.7 |
|
4.8 |
|
4.8A |
|
4.9 |
|
4.10 |
|
10.1 |
|
10.2 |
|
10.3 |
|
10.4 |
|
10.5 |
|
10.6 |
|
10.6A |
I-5
10.6B |
|
10.6C |
|
10.6D |
|
10.6E |
|
10.6F |
|
10.6G |
|
10.6H |
|
10.6I |
|
10.6J |
|
10.6K |
|
10.6L |
|
10.6M |
|
10.6N |
|
10.6O |
|
10.6P |
|
10.6Q |
|
10.6R |
I-6
10.7 |
|
10.8 |
|
10.9 |
|
10.10 |
Form of Annual Amendment to Employment Agreement for the Company’s executive officers. +* |
10.11 |
|
10.12 |
|
21.1 |
|
22.1 |
|
23.1 |
Consent of Independent Registered Public Accounting Firm for Omega Healthcare Investors, Inc.* |
31.1 |
|
31.2 |
|
32.1 |
Section 1350 Certification of the Chief Executive Officer of Omega Healthcare Investors, Inc.* |
32.2 |
Section 1350 Certification of the Chief Financial Officer of Omega Healthcare Investors, Inc.* |
101 |
The following financial statements from the Company’s Annual Report on Form 10-K for the year ended December 31, 2021, formatted in Inline XBRL: (i) Consolidated Balance Sheets, (ii) Consolidated Statements of Operations, (iii) Consolidated Statements of Comprehensive Income, (iv) Consolidated Statements of Changes in Equity, (v) Consolidated Statements of Cash Flows, and (vi) Notes to Consolidated Financial Statements, tagged as blocks of text and including detailed tags. |
104 |
Cover Page Interactive Data File (embedded within the Inline XBRL document and contained in Exhibit 101). |
* Exhibits that are filed or furnished herewith.
+ Management contract or compensatory plan, contract or arrangement.
I-7
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
OMEGA HEALTHCARE INVESTORS, INC. |
||||
Registrant |
||||
Date: |
February 17, 2022 |
By: |
/s/ C. Taylor Pickett |
|
C. Taylor Pickett |
||||
Chief Executive Officer |
||||
I-8
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed by the following persons on behalf of the Omega Healthcare Investors, Inc., for itself and in the capacities on the date indicated.
Signatures |
|
Title |
|
Date |
/s/ C. Taylor Pickett |
Chief Executive Officer |
February 17, 2022 |
||
C. Taylor Pickett |
(Principal Executive Officer) |
|||
/s/ Robert O. Stephenson |
Chief Financial Officer |
February 17, 2022 |
||
Robert O. Stephenson |
(Principal Financial Officer) |
|||
/s/ Neal A. Ballew |
Chief Accounting Officer |
February 17, 2022 |
||
Neal A. Ballew |
(Principal Accounting Officer) |
|||
/s/ Craig R. Callen |
Chair of the Board |
February 17, 2022 |
||
Craig R. Callen |
||||
/s/ Kapila K. Anand |
Director |
February 17, 2022 |
||
Kapila K. Anand |
||||
/s/ Dr. Lisa C. Egbuonu-Davis |
Director |
February 17, 2022 |
||
Dr. Lisa C. Egbuonu-Davis |
||||
/s/ Barbara B. Hill |
Director |
February 17, 2022 |
||
Barbara B. Hill |
||||
/s/ Kevin J. Jacobs |
Director |
February 17, 2022 |
||
Kevin J. Jacobs |
||||
/s/ Edward Lowenthal |
Director |
February 17, 2022 |
||
Edward Lowenthal |
||||
/s/ C. Taylor Pickett |
Director |
February 17, 2022 |
||
C. Taylor Pickett |
||||
/s/ Stephen D. Plavin |
Director |
February 17, 2022 |
||
|
Stephen D. Plavin
/s/ Burke W. Whitman |
Director |
February 17, 2022 |
||
|
Burke W. Whitman
|
I-9